A trial to find the best way of using scans to monitor men after treatment for seminoma testicular cancer (TRISST, MRC TE24)
Cancer type:
Status:
Phase:
This trial was done to find the best way to monitor men who have had treatment for early stage seminoma testicular cancer. It was supported by Cancer Research UK.
The trial was open for people to join between 2008 and 2014, and the team presented the first results at a conference in 2021.
More about this trial
Doctors treat early stage testicular cancer with an operation to remove the testicle. Surgery usually works very well, but there is a small chance the cancer can come back.
When this trial was done, men usually had 7 CT scans in the 5 years after their operation. This is called monitoring, or surveillance. It is important to have scans to pick up any signs that the cancer has come back. But CT scans do expose people to some radiation. This may slightly increase the risk of developing other cancers at a later date.
Doctors wanted to find out if it is safe for men to have CT scans less often, or have MRI scans instead. MRI scans use magnetism to build up a picture, so do not expose people to radiation.
The main aims of this trial were to find out:
- whether it is possible to use MRI scans instead of CT scans to monitor men after surgery for testicular cancer
- how often men should have scans after their operation
Summary of results
The research team found that it was safe for men to have MRI scans instead of CT scans. And that they could have fewer scans.
Trial design
This trial was for men who had stage 1 testicular cancer. They had a type of testicular cancer called seminoma. They had all had surgery to remove their cancer and didn’t need any further treatment.
The people taking part were put into 1 of 4 groups at random. They all had either CT scans or MRI scans after their operation. Some people had 3 scans over 3 years, and some people had 7 scans over 5 years.
The research team followed them up for 6 years after their operation, to see how they were and whether their cancer had come back.
Results
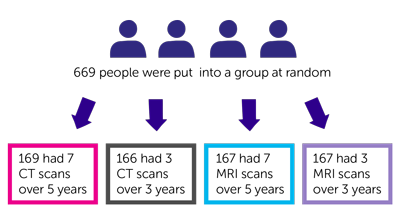
A total 669 people took part in this trial. They were put into a group at random:
- 169 people had 7 CT scans over 5 years
- 166 people had 3 CT scans over 3 years
- 167 people had 7 MRI scans over 5 years
- 167 people had 3 MRI scans over 3 years
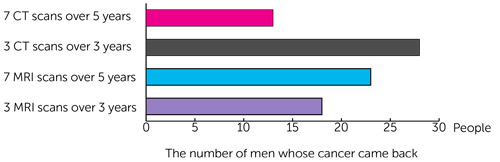
The research team found that the cancer came back in a small number of men in each group, a total of 82 men (12%):
- 13 people who had 7 CT scans over 5 years
- 28 people who had 3 CT scans over 3 years
- 23 people who had 7 MRI scans over 5 years
- 18 people who had 3 MRI scans over 3 years
The cancer came back within 3 years of having surgery in 77 out of the 82 men. It came back later than 3 years after surgery in just 5 men who took part (less than 1%).
For 10 of the men whose cancer came back, the cancer was stage 2C or stage 3. This means it had spread at least one lymph node nearby that was larger than 5cm. Or it had spread to lymph nodes further way, or to another area of the body.
This was the case for:
- 9 men who had 3 scans
- 1 man who had 7 scans
The research team estimate that the cancer may have been picked up at an earlier stage in 4 of the men who had 3 scans, if they had had 7 scans.
The men whose cancer had come back all went on to have more treatment. The cancer went away after this treatment in just over 8 out of 10 men (81%). This is called a complete response.
When the research team did the analysis for the trial in 2020, no one taking part had died because of their cancer.
Conclusion
The trial team concluded that it was safe for men to have fewer scans following surgery for stage 1 seminoma testicular cancer. And that MRI scans could be used instead of CT scans.
They recommend that men in this situation have 3 MRI scans over 3 years, following surgery to remove their cancer.
Where this information comes from
We have based this summary on information from the research team. The information they sent us has been reviewed by independent specialists ( ) but may not have been published in a medical journal. The figures we quote above were provided by the research team. We have not analysed the data ourselves.
) but may not have been published in a medical journal. The figures we quote above were provided by the research team. We have not analysed the data ourselves.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr J. Joffe
Supported by
Cancer Research UK
Experimental Cancer Medicine Centre (ECMC)
Medical Research Council (MRC)
NIHR Clinical Research Network: Cancer
Other information
This is Cancer Research UK trial number CRUK/07/020.
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040