A trial looking at durvalumab for people with non small cell lung cancer after surgery (MERMAID-2)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
This trial is for people with non small cell lung cancer (NSCLC) who:
- have had surgery to completely remove their cancer
- have no sign of cancer on tests and scans after surgery
It is for people who have stage 2 NSCLC, and some people with stage 3 disease.
This trial also looking at measuring small amounts of cancer cells that may be in the bloodstream after surgery. Depending on the results, you may have treatment as part of this trial.
More about this trial
Surgery is a common treatment for stage 2 NSCLC. It is also a treatment option for some people with stage 3 NSCLC.
Some people with NSCLC have a greater risk of their cancer coming back even if:
- surgery was successful
- they had extra cancer treatment before or after surgery
In this situation, doctors usually monitor you with scans to check that there are no signs of cancer. This is called ‘watch and wait’.
Doctors want to improve on ‘watch and wait’. They would like to have a way of finding out whose cancer is more likely to come back.
To do this, they are looking for people with small amounts of cancer  in their blood. This is called
in their blood. This is called  or ctDNA. This could show minimal residual disease (MRD). MRD means that even after successful treatment, there are still some cancer cells releasing DNA into the bloodstream. Because of this, the risk of lung cancer coming back might be higher.
or ctDNA. This could show minimal residual disease (MRD). MRD means that even after successful treatment, there are still some cancer cells releasing DNA into the bloodstream. Because of this, the risk of lung cancer coming back might be higher.
The trial team also want to find out if people in this situation should have treatment with a drug called durvalumab.
Durvalumab is a type of  . It stimulates the body's
. It stimulates the body's  to fight cancer cells.
to fight cancer cells.
Everyone taking part in this trial enters the first surveillance (monitoring for MRD) part of the trial. If MRD is found, this means you are MRD positive.
If you are MRD positive, you have more tests and scans (second screening). You might then go on to have durvalumab or a dummy drug ( ).
).
If no MRD is found, you are MRD negative and have no treatment on the trial.
The main aims of the trial are:
- to learn more about the safety of durvalumab
- to get information about possible side effects of durvalumab
- to see if having durvalumab reduces the risk of cancer coming back
- to learn more about NSCLC and measuring MRD
- to find out more about the
quality of life  of people taking part
of people taking part
Who can enter
The following bullet points are a summary of the entry conditions for the first surveillance part of this trial.
Talk to your doctor or the trial team if you are unsure about any of these. They will be able to advise you. You may be asked to take part in this trial before you have had surgery, or before you have had other treatments after surgery. The following would still need to apply once you have finished all your treatment.
Please note there are also entry conditions for the second screening and treatment part of the trial. The trial team will give you information on this if needed.
Who can take part
You may be able to join this trial if all of the following apply. You:
- have non small cell lung cancer and your cancer has been removed completely with surgery
- have stage 2 or some types of stage 3 cancer (3A and some 3B cancers). Your doctor can explain more.
- have had treatment including surgery alone, or surgery with chemotherapy or
radiotherapy  , which aims to get rid of your cancer completely. Your doctor can explain more.
, which aims to get rid of your cancer completely. Your doctor can explain more. - had CT scans or MRI scans of your tummy (abdomen) and brain before you had surgery. You might need another scan before
randomisation. 
- have had your
lymph nodes  checked for cancer during surgery
checked for cancer during surgery - have a sample of cancer tissue and blood samples that can be sent to the laboratory for
genetic  testing
testing - have had a CT scan of your tummy (abdomen) and brain after surgery, or after
adjuvant treatment  , which showed no cancer in other parts of the body (metastases)
, which showed no cancer in other parts of the body (metastases) - are at least 18 years old
- are willing to use reliable contraception for 90 days after the last dose of the study drug if there is a chance you or your partner could become pregnant. Your doctor will advise you about reliable contraception and when to start using it.
- agree not to donate blood or platelets while taking part in the study and for 90 days after your last dose of durvalumab or until you start another cancer drug
Who can’t take part
Cancer related
You cannot join this trial if any of these apply. You:
- have
EGFR positive  lung cancer or ALK positive lung cancer
lung cancer or ALK positive lung cancer - have a mix of small cell and non small cell lung cancer
- have had another type of cancer in the past. You might still be able to take part if you had treatment to try and get rid of the cancer completely and there has been no sign of cancer in the 5 years before the first dose of the study drug. You might also be able to take part if you have had treated
carcinoma in situ  (CIS) or treated non melanoma skin cancer.
(CIS) or treated non melanoma skin cancer. - have had radiotherapy before surgery (
neoadjuvant  radiotherapy)
radiotherapy) - are having chemotherapy, immunotherapy or targeted cancer drug treatment for another type of cancer
- had radiotherapy treatment to a large area of your body or to over 30% of your bone marrow within the 4 weeks of having your first dose of the study drug
- have had durvalumab or a similar immunotherapy before
Medical conditions
You cannot join this trial if any of these apply. You:
- have active primary
immune deficiency 
- have active
tuberculosis 
- have active hepatitis B or active hepatitis C
- have HIV
- have had medication that dampens down the immune system in the 14 days before your first dose of the study drug. You might still be able to take part if you have had certain types of steroids. Your doctor can explain more.
- have had an organ transplant or
bone marrow transplant  from another person
from another person - have had a
blood transfusion  without removal of white blood cells (leukocytes) in the 120 days before giving your samples for genetic testing
without removal of white blood cells (leukocytes) in the 120 days before giving your samples for genetic testing - have active
autoimmune  or inflammatory disorders, or you have had these in the past. These could include inflammatory bowel disease, diverticulitis or lupus. You might be able to take part if you have vitiligo, alopecia or hypothyroidism. You might also be able to take part if your disorder has not been active in the last 5 years. Your doctor can tell you more.
or inflammatory disorders, or you have had these in the past. These could include inflammatory bowel disease, diverticulitis or lupus. You might be able to take part if you have vitiligo, alopecia or hypothyroidism. You might also be able to take part if your disorder has not been active in the last 5 years. Your doctor can tell you more. - have another illness at the moment that can not be controlled such as an infection, heart problem or a mental health condition. Your doctor can explain more.
- have had major surgery in the 28 days before your first dose of the study drug
Other
You cannot join this trial if any of these apply. You:
- have had a
live vaccine  in the 30 days before your first dose of the study drug
in the 30 days before your first dose of the study drug - are pregnant or breastfeeding
- are allergic to durvalumab or anything it contains
| As well as the above there are specific entry conditions and exclusion criteria for the second screening and treatment part of the trial. Speak to your doctor or research nurse if you want to find out more about the entry conditions for this trial. |
Trial design
This is an international phase 3 trial. The researchers hope that around 1,500 people worldwide will take part. This includes 6 people from the UK having treatment as part of the trial.
First screening and start of surveillance
Everyone taking part has an individual MRD test made for them. To do this, the researchers compare  information in your blood with your cancer tissue sample. This helps them see the difference between your normal blood cells and cancer cells. The team can use this information throughout the trial to see if there are any cancer cells in your blood (MRD).
information in your blood with your cancer tissue sample. This helps them see the difference between your normal blood cells and cancer cells. The team can use this information throughout the trial to see if there are any cancer cells in your blood (MRD).
If you are MRD negative, you are monitored on the trial for nearly 2 years to see if you become MRD positive.
You move onto the second screening part if you are MRD positive:
- at the start of the trial
- at any point during surveillance
Second screening
You have some more tests and scans to see if you are suitable to join the treatment part of the trial. If you are suitable, you move into treatment.
Treatment
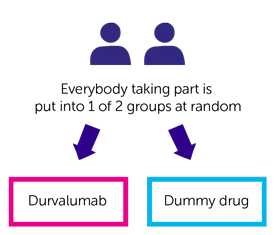
This part of the trial is  . Everyone taking part is put into 1 of the following groups by computer:
. Everyone taking part is put into 1 of the following groups by computer:
- durvalumab (group 1)
- dummy drug (group 2)
Neither you nor your doctor can choose which group you are in. And neither you nor your doctor will know which drug you are having. This is a double blind trial.
You have durvalumab or dummy drug as a drip into your bloodstream (intravenously) every 4 weeks. It takes about 60 minutes to have treatment each time. You continue to have treatment for as long as it is helping you and the side effects aren’t too bad. You can have treatment for up to 2 years.
Follow up
After 2 years, you stop durvalumab or the dummy drug and have regular check ups with your trial doctor until the end of the study.
Quality of life (second screening onwards)
Everyone taking part completes quality of life questionnaires at the time of your second screening and then:
- every 4 weeks for 2 years
- every 4 weeks during follow up – until the end of the study or until your cancer comes back
The questionnaires ask about how you have been feeling and what side effects you have had.
Blood samples
You have blood tests as part of this trial. You have them before the start of treatment and at set times during this trial. Researchers want to:
- find out what happens to durvalumab in your body
- look at the cancer DNA
- look for certain proteins (
biomarkers  ) that can help to tell why some treatments work better than others
) that can help to tell why some treatments work better than others
Tissue sample
The trial team will ask to use a recent tissue sample of your cancer for some tests.
The trial team want to:
- check for the levels of a protein called PD-L1
- check proteins called EGFR and ALK
- look for biomarkers
The team would also like to store this sample for future research. They will give you more information and answer any questions you have.
If your cancer comes back, the trial team would like to take another sample of your cancer. This is to look at why the cancer has returned in more detail. This is optional. You can say no and still take part in the trial.
Hospital visits
You see a doctor and have some tests before taking part. These tests include:
- CT scan or MRI scan of your chest and tummy (abdomen)
- CT scan or MRI scan of your brain
- blood tests
- pregnancy test – if there is any chance you could become pregnant
Tests and scans during monitoring (surveillance)
You have an MRD test every 6 weeks and a CT scan every 12 weeks. This will continue for about 2 years.
Tests and scans during the second screening
You see a doctor and have some tests to see if you are able to join the treatment part of the trial. These tests include:
- CT or MRI scan of your tummy (abdomen) and brain
- heart trace (
ECG  )
) - blood and urine tests
Tests and scans during treatment
You have a CT scan every 8 weeks. You have a blood test before every dose of the study drug. You might have some other tests and scans if your doctor thinks this is needed.
Follow up (MRD negative)
The trial team ask you to take part in an observation period. You don’t have to take part in this. It lasts for up about 2 years.
You visit the hospital around 8 times. You have similar tests as people having usual follow up after lung cancer. These include:
- CT scans every 12 weeks
- blood tests every 8 weeks
After treatment (MRD positive)
After treatment you visit the hospital:
- 4 weeks after you finish treatment
- 12 weeks after you finish treatment
You then see the trial team every 12 weeks for a visit until the study ends.
At each visit the team will catch up with you to see how you are. You have a CT scan or MRI scan at each visit.
Side effects
The trial team monitor you during treatment and afterwards. Contact your advice line or tell your doctor or nurse if any side effects are bad or not getting better.
| Durvalumab can affect the immune system. It may cause inflammation in different parts of the body. This can cause serious side effects. They could happen during treatment, or some months after treatment has finished. Rarely, these side effects could be life threatening. If you have any of these side effects tell your doctor or nurse as soon as possible. You should tell them that you are on or have been on an immunotherapy. |
The most common side effects of durvalumab are:
- diarrhoea
- skin rash or dry, itchy skin
- tummy (abdominal) pain
- a sore throat, runny or stuffy nose – due to an upper respiratory tract infection
- cough
- high temperature (fever)
- your
thyroid gland  not making enough hormone. Symptoms may include tiredness, weight gain, feeling the cold more, constipation, muscle weakness, slow heart rate, puffy face, dry skin, thinning hair and memory problems.
not making enough hormone. Symptoms may include tiredness, weight gain, feeling the cold more, constipation, muscle weakness, slow heart rate, puffy face, dry skin, thinning hair and memory problems.
We have more information on the side effects of durvalumab.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr Yvonne Summers
Supported by
AstraZenca
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040