A trial looking at atezolizumab and chemotherapy for triple negative breast cancer
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
- the hormones oestrogen and progesterone
- the Her 2 protein
More about this trial
- atezolizumab and chemotherapy
- dummy drug (placebo) and chemotherapy
- nab-paclitaxel (Abraxane)
- doxorubicin
- cyclophosphamide
Who can enter
- you have a newly diagnosed triple negative breast cancer and haven’t had any treatment for it
- your cancer measures at least 2 cm across (T2, T3 or T4) and there is no sign that the cancer has spread to other distant parts of the body
- you are willing to have surgery after neoadjuvant therapy
- your heart is working well
- you have satisfactory blood test results
- you have a sample of tissue available that can be used to look for a protein called PD-L1 and to confirm your diagnosis of triple negative breast cancer
- you are able to do everything apart from heavy physical work (performance status 0 or 1)
- you are willing to use reliable contraception during treatment and for up to a year afterwards if there is any possibility that you or your partner could become pregnant
- you are at least 18 years old
- you have had a previous invasive breast cancer
- you have breast cancer in both breasts (bilateral)
- your cancer has spread to other distant parts of the body (metastatic)
- you have had treatment for breast cancer that reached your whole body (systemic)
- you have had atezolizumab, doxorubicin, paclitaxel or any other similar drug
- you have had ductal carcinoma in situ (DCIS) unless you have had surgery to remove the breast (mastectomy) more than 5 years ago
- you have had pleomorphic lobular carcinoma in situ (LCIS) unless you have had surgery for it more than 5 years ago
- you have had an operation to remove the tumour, or a piece of tumour, where the cancer first started (excision or incisional biopsy)
- you have had an operation to remove all the lymph nodes from the armpit or to remove the sentinel lymph node involved with cancer
- you have had another cancer in the last 5 years part from non melanoma skin cancer, an early cancer of the womb, localised prostate cancer, or carcinoma in situ of the cervix that has been successfully treated
- have had a stroke in the last 12 months
- have heart problems such as an irregular heart rhythm (arrhythmia), high blood pressure or angina that isn’t controlled, moderate or severe congestive heart disease, or you have had a heart attack in the last year
- have, or have had, an active autoimmune disease unless it is type 1 diabetes, a thyroid problem called hypothyroidism, or a skin condition called psoriasis, vitiligo or eczema that is stable
- have or have had lung problems such as pneumonitis
- take or have taken drugs that damp down (supress) your immune system such as steroids in the past 2 weeks, unless it was a very small dose or an inhaler
- take or have taken drugs that stimulate the immune system such as interferon in the past 4 weeks
- have HIV
- have hepatitis B or hepatitis C
- have active tuberculosis
- have, or have had a severe infection in the last month
- have taken antibiotics in the last 2 weeks
- have had a major surgery in the last 4 weeks, or doctors think that you will need to have an operation during this trial
- have had an organ transplant from a donor
- have any other medical condition that the trial team think could affect you taking part
- you are sensitive to any of the drugs used in this trial or anything they contain
- have had a live vaccine in the last month
- are pregnant or breastfeeding
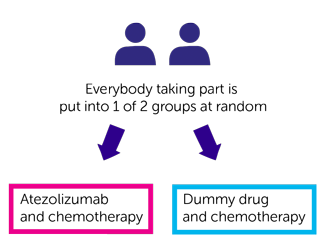
Trial design
- atezolizumab and chemotherapy
- dummy drug and chemotherapy
Atezolizumab or dummy drug
- nab-paclitaxel
- doxorubicin
- cyclophosphamide
- doxorubicin as a drip into your bloodstream every 2 weeks
- cyclophosphamide as a drip into your bloodstream every 2 weeks
- 3 weeks after the start of treatment
- during breast cancer surgery
- if your cancer comes back
- at set times during the trial
- within a month after finishing treatment with atezolizumab or monitoring
- find out what happens to the drugs inside your body (pharmacokinetics)
- look for certain proteins (biomarkers) that can help to tell how well the treatment is working
- look at the cancer DNA
Hospital visits
- a physical examination
- heart trace (ECG)
- a heart scan (MUGA or ECHO)
- blood tests
- urine test
- breast ultrasound
- a lung function test
- a mammogram
Side effects
- tiredness (fatigue) and weakness
- pain in your joints, muscle and bones
- loss of appetite
- loose or watery stools (diarrhoea)
- shortness of breath and cough
- feeling or being sick (vomiting)
- high temperature (fever)
- skin rashes and itching
- bladder infection
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Samreen Ahmed
Supported by
Roche
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040