A trial of cyclophosphamide, dexamethasone and ixazomib for myeloma (MUK 8)
Cancer type:
Status:
Phase:
This trial was for people whose myeloma had come back or whose treatment had stopped working.
The trial was open for people to join between 2016 and 2018. The team published some results in 2022.
More about this trial
When this trial was done, the usual treatments for myeloma included cyclophosphamide and the steroid drug dexamethasone. People had these on their own or alongside 1 of the following:
- thalidomide
- lenalidomide
- a drug called a proteasome inhibitor such as bortezomib (Velcade) or carfilzomib (Kyprolis)
In this trial researchers were looking at a drug called ixazomib alongside cyclophosphamide and dexamethasone. Ixazomib is a type of targeted cancer drug. It is a cancer growth blocker. It stops signals that cancer cells use to divide and grow.
The researchers wanted to find out if having ixazomib as well could help stop the cancer coming back.
Everyone taking part in this trial had myeloma that had come back after  .
.
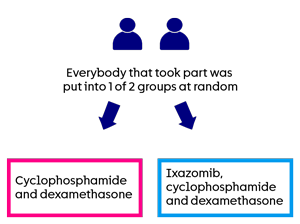
This was a phase 2 trial. People taking part were put into one of 2 groups at random:
- half had cyclophosphamide and dexamethasone (CD)
- half had ixazomib, cyclophosphamide and dexamethasone (ICD)
The main aims of the trial were to find out:
- if ixazomib helps stop myeloma coming back
- more about the side effects
Summary of results
The research team found that having ixazomib with cyclophosphamide and dexamethasone did not help stop myeloma coming back. This was for people who had already had treatment for their myeloma.
Results
The research team hoped that about 250 people would join this trial. But they found it harder than they expected to find people to take part in this trial. So it closed earlier than planned.
A total of 112 people joined the trial. A computer put people taking part into 1 of 2 groups at random. There were
- 58 people in the ixazomib, cyclophosphamide and dexamethasone (ICD) group
- 54 people in the cyclophosphamide and dexamethasone (CD) group
A total of 110 people had treatment as part of this trial. The research team analysed the results in 2019.
They looked at how many people’s myeloma had got a bit better. They found it was:
- 24 out of 57 people (42%) who had ICD
- 21 out of 53 people (40%) who had CD
The also looked how long it was before people’s myeloma started to get worse. They found this was:
- 5.6 months for those who had ICD
- 6.7 months for those who had CD
They looked at the time until half the people in each group were living. They call this median overall survival. They found it was:
- about 14 months for those who had ICD
- about 19 months for those who had CD
The results for the two groups look different, but there is not a big enough difference to say for sure that it’s due to the treatment. It could be due to chance.
Quality of life
The researchers also looked at the quality of life of people taking part. They asked people to complete questionnaires at regular times during treatment. These asked how people were feeling and about any problems they were having.
They found that the quality of life in the two groups was similar at the start of the trial and at 3 months.
At 6 months, people in the CD group had a slightly higher quality of life compared to those in the ICD group.
Side effects
Most people (98%) who took part had at least one side effect from treatment. But many were mild or didn’t last long.
The most common side effects were:
- a drop in red blood cells causing shortness of breath and tiredness
- a drop in blood clotting cells (platelets) causing bruising or bleeding problems
- severe tiredness (fatigue)
- diarrhoea
- a drop in white blood cells causing an increased risk of infection
- infection
Some people had more severe side effects. This was:
- 34 people (60%) who had ICD
- 26 people (49%) who had CD
More people who had ICD had:
- a drop in white blood cells causing an increased risk of infection
- diarrhoea
- nerve changes in their hands and feet such as numbness or pins and needles
- extreme tiredness (fatigue)
- infection
- a drop in blood clotting cells (platelets) causing bruising or bleeding
More people who had CD had:
- low blood pressure
- high blood sugar
- a drop in red blood cells causing shortness of breath and tiredness
Some people decided to stop treatment because of side effects they were having. This was:
- 8 people in the ICD group
- 5 people in the CD group
Three people who had ICD died because of side effects from treatment. Two people had a serious infection. And one had bleeding in the brain. No one who had CD died because of side effects from treatment.
The trial team concluded that ixazomib, cyclophosphamide and dexamethasone did not work better than cyclophosphamide and dexamethasone. This is for people who’d already had treatment for their myeloma but it had come back.
Sometimes trials show a different combination of treatment isn’t useful for a particular type or  of cancer. But these trials still add to our knowledge and understanding of cancer and how to treat it.
of cancer. But these trials still add to our knowledge and understanding of cancer and how to treat it.
More detailed information
There is more information about this research in the reference below.
Please note, the information we link to here is not in plain English. It has been written for healthcare professionals and researchers.
Ixazomib with cyclophosphamide and dexamethasone in relapsed or refractory myeloma: MUKeight phase II randomised controlled trial results
H Auner and others
Blood Cancer Journal, 2022. Volume 12, Issue 52
Where this information comes from
We have based this summary on the information in the article above. As far as we are aware, this has been reviewed by independent specialists ( ) and published in a medical journal. We have not analysed the data ourselves. As far as we are aware, the link we list above is active and the article is free and available to view.
) and published in a medical journal. We have not analysed the data ourselves. As far as we are aware, the link we list above is active and the article is free and available to view.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Gordon Cook
Supported by
Myeloma UK
NIHR Clinical Research Network: Cancer
Takeda Oncology
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040