A study looking at outcome measures in palliative care
Cancer type:
Status:
Phase:
This study looked at what people thought about using questionnaires to assess the needs and plan the treatment of people needing palliative care.
More about this trial
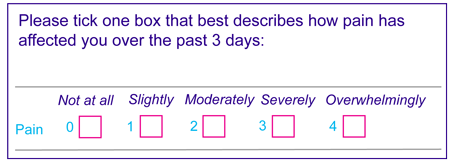
Outcome measures are a way of finding out what is important to patients and how they are doing. Issues in palliative care may include pain, loss of appetite, shortness of breath, constipation, anxiety or depression.
This pain scale is an example of an outcome measure that could be used to monitor pain. The scale uses numbers to assess how much the pain has affected people recently. It goes from 0 (not at all) to 4 (overwhelmingly).
- whether they would be willing to use outcome measures
- what difference they think using outcome measures could make
Summary of results
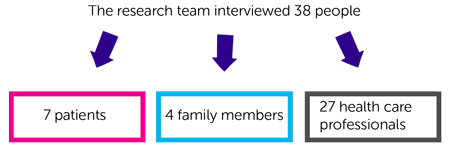
- 7 patients
- 4 family members
- 27 health care professionals
- a better understanding of specific needs or issues for individual patients
- better assessment and monitoring of care
- improved communication between patients, carers and health care professionals
- patients and their families feeling more involved in care, and finding it easier to feedback to the health care team
- an increase in pressure on the time of health care professionals
- some people may have issues that are not included in the questionnaires
- difficulty completing the questions when patients are very poorly
- no guarantee it would improve care
 ) and published in a medical journal. See reference section below for more details. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
) and published in a medical journal. See reference section below for more details. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
Reference
Perspectives of patients, family caregivers and health professionals on the use of outcome measures in palliative care and lessons for implementation: a multi-method qualitative study.
Catherine Pinto, Fliss Murtagh and others
Annals of Palliative Medicine, volume 7, supplement 3, pages 137 - 150
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr Fliss Murtagh
Supported by
Guy's & St Thomas' Charity
King's College London
NIHR Clinical Research Network: Cancer
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040