A trial looking at irosustat to treat advanced womb cancer
Cancer type:
Status:
Phase:
- had been through the
menopause 
- had womb cancer that is sensitive to the female hormone oestrogen (
oestrogen receptor positive  or ER positive)
or ER positive) - could not have surgery or radiotherapy
More about this trial
- find out if irosustat worked better than megestrol acetate 6 months after treatment started
- learn more about the side effects
Summary of results
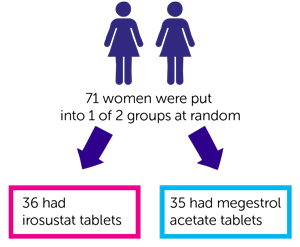
- 36 had irosustat tablets
- 35 had megestrol acetate tablets
- just under 4 out of 10 women (36%) who had irosustat
- just over 5 out of 10 women (54%) who had megestrol acetate
- in 3 women the cancer went away a little bit
- in 17 women the cancer stayed the same
- in 14 women the cancer got worse
- they didn’t have the results for 1 woman
- in 2 women the cancer went away completely
- in 10 women the cancer went away a little bit
- in 12 women the cancer stayed the same
- in 8 women the cancer got worse
- they didn’t have the results for 2 women
The researchers also looked at the average length of time before the cancer started to grow again. On average this was:
- 16 weeks in women who had irosustat
- 40 weeks in women who had megestrol acetate
- how well the cancer responded to treatment
- how long women lived for
 ) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr John Green
Supported by
Experimental Cancer Medicine Centre (ECMC)
Ipsen
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040