A study of 2 different combinations of chemotherapy before surgery for cancer of the pancreas (PRIMUS 002)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
More about this trial
- FOLFOX and nab-paclitaxel (FOLFOX-A)
- gemcitabine and nab-paclitaxel (AG)
- fluorouracil (5FU)
- oxaliplatin
- nab-paclitaxel
- find the best way to treat localised pancreatic cancer
- predict who benefits most from chemotherapy before surgery
- learn more about the side effects of treatment
Who can enter
- you have joined the Precision-Panc study and there are some suitable tissue samples available for the study team to do some tests on
- you have a type of pancreatic cancer called ductal adenocarcinoma
- your cancer can be measured on a scan
- you can have surgery to remove the cancer
- you are fit enough to have surgery, chemotherapy and chemoradiotherapy
- it is possible to have a metal tube inserted into your bile duct if you develop a condition called jaundice
- you are well enough to carry out all your normal activities, apart from heavy physical work (performance status 0 or 1)
- you are willing to use reliable contraception during treatment and for 6 months afterwards if there is any chance you or your partner could become pregnant
- you have satisfactory blood test results
- you are at least 16 years old
- have cancer that has spread elsewhere in the body
- have had any other cancer apart from basal cell skin cancer or early cervical cancer that has been successfully treated
- have already had chemotherapy or chemoradiotherapy for pancreatic cancer
- have had an experimental treatment that hasn’t completely cleared your body
- have a heart problem that isn’t controlled with medication
- have an infection including chicken pox or herpes
- are overweight (body mass index of more than 35)
- have long term liver disease unless your liver is still working normally (Child-Pugh A)
- have had an exercise test that shows you aren’t a suitable candidate for surgery
- have had major surgery in the last 28 days
- have very bad diarrhoea that isn’t controlled with medication
- have had problems with the digestive system called malabsorption
- have a condition called DPD (stands for dihydropyridine dehydrogenase which means you can’t break down chemotherapy properly)
- have moderate to severe numbness or tingling in your hands or feet
- are having any antiviral treatment such as brivudine or sorivudine
- have a mental health problem or any other serious medical condition that means you can’t take part in the study
- are sensitive to any of the study drugs
- are pregnant or breastfeeding
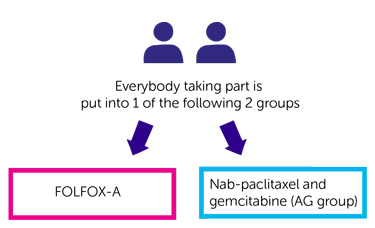
Trial design
- FOLFOX-A
- nab-paclitaxel and gemcitabine (AG group)
You have all your treatment as a drip into a vein. You have chemotherapy in cycles.
- day 1
- day 8
- day 15
- when you join the Precision-Panc study
- during surgery
Hospital visits
- blood tests
- physical examination
- heart trace (ECG)
- CT scan
- MRI scan of your liver
- an exercise test to check your heart and lung function
- for blood tests
- a physical examination
- to see how you are
- every 3 months in the 1st year
- every 6 months after that
Side effects
- a drop in the number of blood cells causing an increased risk of infection, bleeding problems, tiredness and breathlessness
- feeling or being sick
- skin rash
- numbness or tingling in your hands or feet
- fluid loss (dehydration)
- hair loss or thinning
- tiredness (fatigue)
- headache
- shortness of breath
- cough
- nose bleeds
- stomach pain
- taste changes
- swelling
- dizziness
- fever or chills
- weight loss
- depression
- difficulty sleeping
- loss of appetite
- low levels of potassium in the blood
- liver changes
- a sore mouth
- an unpleasant sensation in the throat
- diarrhoea or constipation
- redness, swelling and pain on the palms of your hands and soles of your feet (palmar plantar syndrome)
- an allergic reaction, including a skin rash
- pain, swelling or sores on the inside of the mouth
- flu like symptoms
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr Derek Grose
Supported by
Cancer Research UK
Cancer Research UK Clinical Trials Unit, Glasgow
NHS Greater Glasgow and Clyde
Celgene
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040