A trial of atezolizumab for urothelial cancer (urinary tract cancer) after surgery (W029636)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
This trial is for people whose cancer has grown into the muscle layer of the bladder or upper urinary tract (invasive urothelial cancer). And whose cancer hasn't spread elsewhere in the body.
The urinary tract includes the:
- centre of the kidney (renal pelvis)
- tube that takes urine from the kidneys to the bladder (ureter)
- bladder
More about this trial
Removing the bladder (a cystectomy) or the kidney and ureter (a nephroureterectomy) is the usual treatment for invasive urothelial cancer.
You are then followed up to see if there are any signs of the cancer coming back. In this trial, researchers want to see if having atezolizumab after surgery delays or prevents the cancer coming back.
Atezolizumab (also known as MPDL3280A) is an  . It works by affecting a substance called PD-L1. When cancer cells have a lot of PD-L1 on their surface, the immune system doesn’t work properly in getting rid of them.
. It works by affecting a substance called PD-L1. When cancer cells have a lot of PD-L1 on their surface, the immune system doesn’t work properly in getting rid of them.
Atezolizumab blocks the way PD-L1 works (the PD-L1 pathway) and so could help your immune system to stop or shrink the cancer growth.
If a cancer has large amounts of PD-L1, it is described as being PD-L1 positive. To be able to take part in this trial you must be PD-L1 positive. Your doctors will test for this.
Some people in this trial have atezolizumab after surgery. The other group don’t have treatment and are followed up as usual.
The aims of this trial are to
- find out how well atezolizumab works for people after surgery for urothelial cancer
- learn more about the side effects
Who can enter
The following bullet points list the entry conditions for this trial. Talk to your doctor or the trial team if you are unsure about any of these. They will be able to advise you.
You may be able to join this trial if all of the following apply.
- You have transitional cell bladder cancer or upper urinary tract cancer and
-
You have cancer that has grown into the muscle layer of the bladder or beyond (stage T2 to T4a) or it has spread into the lymph nodes and you had chemotherapy before surgery OR
- You have cancer that has grown through the muscle and outside of the bladder (stage T3 –T4a) or into the lymph nodes and you didn’t have chemotherapy before surgery
-
- You have had a cystectomy or nephroureterectomy, your lymph nodes removed and the surgeons were able to remove all of the cancer
- There are enough samples of your cancer available for the trial team to do some tests
- If you didn’t have chemotherapy before surgery, there is a reason why you might not be able to have cisplatin chemotherapy afterwards. For example you aren’t well enough or your kidneys aren’t working properly
- You have fully recovered within 14 weeks of having surgery
- You are well enough to be up and about for at least half the day (performance status of 0, 1 or 2)
- You have satisfactory blood test results
- You are willing to use reliable contraception during treatment and for 5 months afterwards if there is any chance that you or your partner could become pregnant
- You are at least 18 years old
You cannot join this trial if any of these apply. You
- Have bladder cancer that has spread to another part of the body
- Have already had a drug that targets PD-1, PD-L1, CD137, CD40 or CTLA-4 such as ipilimumab, nivolumab or pembrolizumab
- Have had any other cancer treatment in the 3 weeks before starting treatment in this trial
- Have had treatment that stimulates the immune system such as interferon or IL-2 in the last 6 weeks before joining the trial
- Have had steroid treatment in the 2 weeks before joining the trial
- Have an
autoimmune disease  such as rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, myasthenia gravis. If you have a condition of auto immune related hypothyroidism and are on a stable dose of thyroid replacement hormone you may be able to take part in the trial. And if you have type 1 diabetes and are on a stable dose of insulin you might also be able to take part.
such as rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, myasthenia gravis. If you have a condition of auto immune related hypothyroidism and are on a stable dose of thyroid replacement hormone you may be able to take part in the trial. And if you have type 1 diabetes and are on a stable dose of insulin you might also be able to take part. - Have a lung condition called interstitial lung disease
- Have problems with your heart, such as a heart attack in the last 3 months, angina that is not well controlled or an abnormal rhythm of your heart
- Have had any other cancer in the last 5 years, apart from low risk prostate cancer or certain cancers that were very early stage and have been successfully treated such as
non melanoma skin cancer  or CIS of the cervix
or CIS of the cervix - Have had a
stem cell transplant  with someone else’s cells or an organ transplant
with someone else’s cells or an organ transplant - Have had an allergic reaction to atezolizumab or you are sensitive to any drugs that are similar or that are produced in a similar way
- Have been in hospital with a serious infection in the 4 weeks before starting trial treatment or you have had any signs or symptoms of a serious infection in the last 2 weeks
- Have had antibiotics in the last 2 weeks before joining the trial
- Are HIV positive
- Have an active hepatitis B or hepatitis C infection
- Have tuberculosis (TB) causing symptoms
- Have had major surgery in the last month
- Have had a
live vaccination  in the last month
in the last month - Have had any other experimental treatment as part of a clinical trial in the last 4 weeks
- Have any other medical condition or mental health problem that the trial team think would affect you taking part in this trial
- Are pregnant or breastfeeding
Trial design
This international phase 3 trial needs about 25 people from the UK to take part.
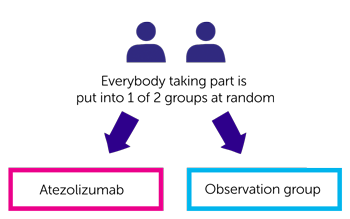
The trial is randomised. You are put into 1 of 2 treatment groups by computer. Neither you nor your doctor will be able to decide which group you are in.
The people taking part are put into 1 of 2 groups.
- One group have atezolizumab
- The other group don’t have treatment (this is called the observation group)
In the atezolizumab group, you have treatment once every 3 weeks. You have it as a drip into a vein. It takes about an hour each time. You continue having treatment for up to a year as long it is helping you and the side effects aren’t too bad.
In the observation group you see the trial team every 3 weeks for a year or they will phone you at home to see how you are getting on. This is the usual way of following people up after upper urinary tract cancer surgery who are not able to have cisplatin chemotherapy.
Research samples
The researchers will ask for a sample of your cancer that was removed when you had surgery or a  . They will use these samples to better understand bladder cancer and find out why some people don’t respond to some treatments.
. They will use these samples to better understand bladder cancer and find out why some people don’t respond to some treatments.
They will also ask to take extra blood and urine tests as part of this trial to look for  .
.
You don’t have to give these extra samples if you don’t want to. You can still take part in the trial.
Hospital visits
You see trial doctors and have some tests before you start treatment. These include
You might also have a scan of the kidneys and the tubes draining the kidneys called the ureters.
You have regular scans while you are taking part in the trial. When the trial finishes, you have a CT or MRI scan every
- 3 months for the first 3 years
- 6 months for the following 3 years
The trial team will contact you by phone every 3 months for up to 6 years to see how you are getting on.
Side effects
As atezolizumab is a new drug there may be some side effects we don’t know about yet. The trial team will monitor you during the time you have treatment and you will be given a phone number to call them if you are worried about anything.
So far, the most common side effects include
- tiredness (fatigue)
- cough
- diarrhoea or constipation
- feeling or being sick
- loss of appetite
- headache
- chills
- a drop in red blood cells causing tiredness and breathlessness
- fever
- difficulty sleeping
- muscle pain, joint pain, tummy (abdominal) and back pain
- hair loss
- skin rash
- shortness of breath
- swelling of the hands and feet
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr Alison Birtle
Supported by
Experimental Cancer Medicine Centre (ECMC)
Roche
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040



