A trial of talimogene laherparepvec and pembrolizumab for advanced melanoma (MASTERKEY-265)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
This trial is for people with melanoma skin cancer that cannot be removed by surgery or that has spread to other parts of the body (advanced melanoma).
More about this trial
Melanoma is often treated with surgery. But sometimes it cannot be completely removed or it spreads to other parts of the body. This is called advanced melanoma.
Researchers are looking for new treatments to help people in this situation. In this trial, they are looking at 2 drugs:
- talimogene laherparepvec (also called Imlygic)
- pembrolizumab (also called Keytruda)
Talimogene laherparepvec is a form of the cold sore  (herpes simplex). It has been changed so it can make a protein called human granulocyte macrophage colony stimulating factor (GM-CSF).
(herpes simplex). It has been changed so it can make a protein called human granulocyte macrophage colony stimulating factor (GM-CSF).
GM-CSF is a growth factor. It is naturally made by the body to help the immune system recognise and attack cancer cells.
Researchers think talimogene laherparepvec works in 2 ways:
- puts the virus into cancer cells where it can attack them
- helps the immune system to recognise and attack cancer cells
Pembrolizumab is a type of biological therapy called monoclonal antibody. It helps your immune system to attack the cancer and stop it from growing.
This drug is already used to treat people with advanced melanoma but this is the first time talimogene laherparepvec and pembrolizumab will be given together.
In this trial, people have 1 of the following:
- talimogene laherparepvec and pembrolizumab
- dummy drug (
Placebo  ) and pembrolizumab
) and pembrolizumab
The aims of this trial are to:
- find out how well talimogene laherparepvec and pembrolizumab work together as a treatment
- learn more about the side effects
- learn how well people cope with side effects
- find out what happens to talimogene laherparepvec and pembrolizumab in the body (
pharmacokinetics  )
)
Who can enter
The following bullet points list the entry conditions for this trial. Talk to your doctor or the trial team if you are unsure about any of these. They will be able to advise you.
You may be able to join this trial if all of the following apply. You:
- Have melanoma that has spread to other parts of the body and cannot be completely removed by surgery (stage 3b to stage 4)
- Have 1 area of melanoma at least 10 mm across (diameter) that talimogene laherparepvec can be injected into or have a number of smaller areas of melanoma that can be injected into and the total of the diameters of each area adds up to at least 10 mm
- Have at least 1 area of cancer that can be measured on a scan
- Are willing to have a sample of your cancer taken (a
biopsy  ) if there is no suitable sample available that is less than 3 months old. The biopsy must not have been taken within 3 months of any treatment that reached your whole body (
) if there is no suitable sample available that is less than 3 months old. The biopsy must not have been taken within 3 months of any treatment that reached your whole body (systemic treatment  )
) - Have satisfactory blood tests results
- Are well enough to carry out your normal activities, apart from heavy physical work (performance status of 0 or 1)
- Are at least 18 years old
- Are willing to use reliable contraception during treatment and for 3 months after the final dose of talimogene laherparepvec or 4 months after the last dose of pembrolizumab if there is any possibility you or your partner could become pregnant and are willing to use male or female latex condoms during treatment and for 30 days afterwards to avoid the possibility of passing on talimogene laherparepvec
If you have contact with people who have a weakened immune system, have HIV and are pregnant or with children under 1 year, you must take precautions against exposing them to your blood and other bodily fluids (such as your saliva, urine or semen) during the time you have treatment with talimogene laherparepvec and for 28 days afterwards.
You cannot join this trial if any of these apply. You:
- Have melanoma that started in the eye (uveal melanoma) or in the mucosal tissue (
mucosal melanoma  )
) - Developed melanoma after having an organ transplant, leukaemia or you were born with a problem with your immune system and the doctors think your melanoma is linked to these conditions
- Have melanoma spread to the brain that hasn’t been treated (you may be able to join if you have no more than 3 areas of melanoma spread to the brain, have had treatment with surgery,
gamma knife therapy  or
or stereotactic radiotherapy  , there is no sign of the areas growing and you haven’t needed steroids for the past 2 months)
, there is no sign of the areas growing and you haven’t needed steroids for the past 2 months) - Are due to have any other anti cancer treatment during the time of the trial apart from radiotherapy to manage symptoms (palliative radiotherapy)
- Have had talimogene laherparepvec or any other virus (oncolytic viruses) to treat your cancer
- Have had pembrolizumab or any other similar drug such as nivolumab
- Have had an experimental drug or used an experimental device as part of another clinical trial in the past 28 days
- Have had radiotherapy in the past 28 days
- Have had a cancer drug called interferon, a monoclonal antibody (such as ipilimumab) or chemotherapy given into your arm or leg (regional chemotherapy) in the past 28 days
- Have moderate to severe side effects from previous anti cancer treatments
- Have had a stem cell transplant in the last 5 years using donor stem cells
- Have had a cancer vaccine
- Have had another cancer in the past 3 years apart from successfully treated early cancer (
carcinoma in situ  ) of the cervix, breast, prostate or bladder, successfully treated non-melanoma skin cancer or any other cancer treated with the aim to cure, no signs of it for at least 3 years and a low risk of it coming back
) of the cervix, breast, prostate or bladder, successfully treated non-melanoma skin cancer or any other cancer treated with the aim to cure, no signs of it for at least 3 years and a low risk of it coming back - Have or have had an
autoimmune disease  such as autoimmune pneumonitis, glomerulonephritis, vasculitis or any other autoimmune condition that is causing symptoms or needed treatment that reached your whole body (systemic treatment) in the past 2 years (unless it is vitiligo, childhood asthma that has resolved, thyroid problems that are controlled by medications or treatment that replaces something in the body such as insulin)
such as autoimmune pneumonitis, glomerulonephritis, vasculitis or any other autoimmune condition that is causing symptoms or needed treatment that reached your whole body (systemic treatment) in the past 2 years (unless it is vitiligo, childhood asthma that has resolved, thyroid problems that are controlled by medications or treatment that replaces something in the body such as insulin) - Have a weakened immune system due to another disease such as infection
- Have taken drugs that damp down your immune system (immunosuppressants) such as steroids in the past 7 days or for more than 2 weeks (unless it was an inhaler)
- Have an herpes infection or a skin lesion (herpetic skin lesion) that needs treatment (such as acyclovir) by mouth or as an injection (the occasional use of creams may be allowed)
- Have had complications caused by herpes infection such as inflammation of the eye (herpetic keratitis) or the brain (encephalitis)
- Are known to be sensitive to talimogene laherparepvec, pembrolizumab or anything it contains
- Have had a live
vaccination  in the past 28 days
in the past 28 days - Have HIV
- Have hepatitis B or hepatitis C
- Have active tuberculosis (TB)
- Have any other serious medical condition or mental health problem that the trial team think could affect you taking part
- Are pregnant or breast feeding
In some people, their melanoma might have changes to the BRAF  . If your melanoma is either BRAF wild type or has a BRAF mutation there are some treatments you either cannot have had before starting treatment in this trial or you must have finished the treatment in the last 2 weeks and have recovered from any side effects. The trial team can give you more details.
. If your melanoma is either BRAF wild type or has a BRAF mutation there are some treatments you either cannot have had before starting treatment in this trial or you must have finished the treatment in the last 2 weeks and have recovered from any side effects. The trial team can give you more details.
Trial design
This is an international phase 3 trial. The researchers need about 660 people worldwide and around 21 people in the UK to take part.
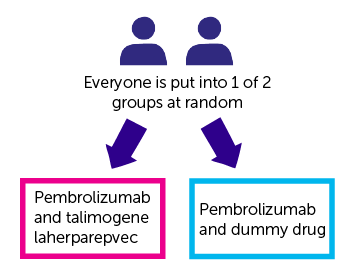
This trial is randomised. The people taking part are put into 1 of the following treatment groups by computer:
- pembrolizumab and talimogene laherparepvec
- pembrolizumab and dummy drug (placebo)
Neither you or your doctor are able to decide which group you are in. And neither you or your doctor will know which group you are in. This is common in clinical trials and is called a  .
.
Everyone taking part has pembrolizumab. You have it as a drip into a vein every 3 weeks. It takes about 30 minutes.
You continue to have pembrolizumab for as long as your cancer doesn’t get worse and the side effects aren’t too bad. You can have up to 2 years.
You have either talimogene laherparepvec or the dummy drug in the same way. You have an injection directly into the melanoma in the skin or the lymph nodes. You may have more than 1 melanoma site injected. Your doctor will explain how many sites will be injected.
The doctor might use an  to guide the injections.
to guide the injections.
You have the first injection just before your pembrolizumab. You have the next injection 3 weeks later and then every 2 weeks until the 5th injection. You then have it every 3 weeks.
You continue having talimogene laherparepvec or the dummy drug for:
- as long as it is helping
- you have lesions to inject
- the side effects aren’t too bad
You can have up to 2 years.
Quality of life
Everybody taking part of this trial will be asked to complete a quality of life questionnaire before starting treatment, at set times during the trial and then after you finish your treatment.
It will ask about how you have been feeling and what side affects you have had.
Blood tests
You have some extra blood tests as part of this trial. The researchers want to find out what happens to talimogene laherparepvec and pembrolizumab in the body (pharmacokinetics).
They will also look for substances called  to see why treatment works better for some people than others.
to see why treatment works better for some people than others.
Researchers will ask to store your blood samples for up to 20 years and use them in future studies. You do not have to agree to have your blood stored if you don’t want to. You can still take part in the trial.
Tissue sample
You might need to give a tissue sample (biopsy) of your cancer before you start treatment. This is to:
- check if there is a marker on your cancer called PD-L1
- check if there is a change in the BRAF gene
- look for biomarkers to see why treatment works better for some people than others
Researchers can use a tissue sample of your cancer taken less than 3 months ago. You must have completed any treatment that reached your whole body (systemic treatment) more than 3 months before you had the biopsy.
If there is not a suitable sample available, you need to have a biopsy.
You also need to have new tissue samples taken:
- before the 5th injection of talimogene laherparepvec or dummy drug
- if your cancer gets worse (this is only for the first 100 people)
Photographs
You have photos of your melanoma taken as part of this trial. The research team takes up to 5 photos before the start of treatment and then every 12 weeks.
Cold sores
Talimogene laherparepvec uses a form of the cold sore vires (herpes simplex). So it could cause cold sores.
If this happens, the research team will take a swab of the lesion to check if it is caused by the talimogene laherparepvec.
Hospital visits
You see a doctor and have some tests before taking part. These tests include:
You see the doctor and have blood tests every 3 weeks.
You have a CT, PET-CT or an MRI scan every 12 weeks while you are having treatment.
This continues for as long as your cancer stays the same and does not get worse. If your cancer gets worse you stop having pembrolizumab and talimogene laherparepvec or dummy drug
When you finish your treatment you see the doctor after 1 month. You have blood tests and a physical examination.
You then see the trial team every 3 months. They can phone you instead to see how you are.
This continues for about 5 years. At the end, the researchers find out if you had talimogene laherparepvec or the dummy drug.
If you had talimogene laherparepvec, the researchers will ask if you want to take part in a long term follow up study called the registry study.
The researchers phone you every 3 months. They ask you how you are, if you have been in hospital, any new illness you may have had and what medications you take.
You don’t have to agree to the registry study if you don’t want to. You can still take part.
Side effects
The trial team monitor you during the time you have treatment and you will be given a phone number to call them if you are worried about anything. The team will tell you about all the possible side effects before you start the trial.
The most common side effects of talimogene laherparepvec are:
- flu like symptoms such as chills, a high temperature (fever), feeling or being sick, tiredness (fatigue) and muscle pain
- pain at the injection site
- headache
- joint, arm and leg pain
- diarrhoea or constipation
We have information about pembrolizumab.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Kevin Harrington
Supported by
Amgen
Experimental Cancer Medicine Centre (ECMC)
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040



