A trial looking at nivolumab for people with advanced liver cancer (CA209459)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
This trial is for people with a type of liver cancer called hepatocellular carcinoma (HCC) that can’t be removed by surgery. It is for people who have not had treatment that reaches the whole body ( ).
).
More about this trial
Doctors can use a number of different treatments for HCC. But sometimes the cancer can get worse or come back. If this happens it is called  .
.
The  for people with advanced liver cancer is a drug called sorafenib.
for people with advanced liver cancer is a drug called sorafenib.
Sorafenib is a type of biological therapy called a tyrosine kinase inhibitor (TKI). It works in 2 ways
- blocks the signals that tell cancer cells to grow
- stops cancer cells from making blood vessels (which they need to grow)
In this trial doctors are looking at a drug called nivolumab. It is a different type of biological therapy called a monoclonal antibody. Researchers think nivolumab can help your immune system attack your cancer and stop it from growing.
In this trial, people will have 1 of the following
- nivolumab
- sorafenib
The aims of this trial are to
- find out how well nivolumab work as a treatment
- find out what happens to nivolumab in your body
- find out why treatments work better for some people than others
- learn more about side effects
- learn how well people cope with side effects
Who can enter
The following bullet points list the entry conditions for this trial. Talk to your doctor or the trial team if you are unsure about any of these. They will be able to advise you.
You may be able to join this trial if all of the following apply
- You have hepatocellular carcinoma that has got worse and cannot be cured by surgery (or by any other treatments given directly to the liver such as radiofrequency ablation, chemoembolization or alcohol injections into the liver)
- You are willing to have a sample of your cancer taken (a
biopsy  ) if there is no suitable sample available
) if there is no suitable sample available - You have at least 1 area of cancer that hasn’t been treated, can be seen on a scan and measures at least 10 mm
- You have satisfactory blood tests results
- Your heart is working well
- Your liver is working normally (Child-Pugh grade A)
- You are well enough to carry out your normal activities, apart from heavy physical work (performance status of 0 or 1)
- You are able to swallow tablets
- You are at least 18 years old
- You are willing to use reliable contraception during treatment and for 23 weeks after the final dose of nivolumab if you are a women, or 31 weeks if you are a man, if there is any possibility you or your partner could become pregnant. If you have sorafenib, the trial team will advise you how long you should use reliable contraception for
You cannot join this trial if any of these apply
- You have a type of liver cancer called fibrolamellar HCC, sarcomatoid HCC or mixed cholangiocarcinoma and HCC
- Your cancer has spread to your brain, tissues surrounding your brain or your
spinal cord  . You might still be able to take part if you have had surgery or radiotherapy more than 28 days ago, it has not got worse in the past 4 weeks and you are no longer taking steroids
. You might still be able to take part if you have had surgery or radiotherapy more than 28 days ago, it has not got worse in the past 4 weeks and you are no longer taking steroids - You have had another cancer in the last 3 years apart from successfully treated early cancers (
carcinoma in situ  ) of the prostate, cervix or breast or successfully treated basal or squamous cell skin cancer
) of the prostate, cervix or breast or successfully treated basal or squamous cell skin cancer - You have had treatment that reached the whole body (systemic treatment)
- You have had treatment given directly into the liver such as radiofrequency ablation, chemoembolization or alcohol injections in the past 4 weeks
- You have had radiotherapy in the last 4 weeks (2 weeks if this was to control symptoms - palliative radiotherapy)
- You have moderate to severe side effects from previous anti cancer treatments
- You have had major surgery in the last 4 weeks or a minor surgery such as biopsy or
FNA  in the past week
in the past week - You have had an organ transplant (including liver or
bone marrow  transplant)
transplant) - You have problems with your
thyroid  that are not controlled by medication
that are not controlled by medication - You have lung problems such as interstitial lung disease
- You have heart problems such as congestive heart failure, high blood pressure that is not controlled by medication, valvular heart disease, angina that is not controlled or a heart attack in the past 6 months
- You have problems with your
digestive system  such as malabsorption syndrome or an active lesion (peptic ulcer) in the lining of the stomach or the food pipe (oesophagus)
such as malabsorption syndrome or an active lesion (peptic ulcer) in the lining of the stomach or the food pipe (oesophagus) - You have an
autoimmune disease  unless it is vitiligo, type 1 diabetes, childhood asthma that has been resolved, thyroid problems that are controlled by medications or a skin condition called psoriasis that doesn’t need treatment
unless it is vitiligo, type 1 diabetes, childhood asthma that has been resolved, thyroid problems that are controlled by medications or a skin condition called psoriasis that doesn’t need treatment - Your liver doesn’t work well and has made you confused as a result (hepatic encephalopathy) – the doctor will check for this
- You have a build up of fluid in the abdomen (ascites) that isn’t controlled by treatment
- You have had bleeding from swollen veins (varices) in the stomach or food pipe (oesophagus) in the last 6 months
- You have taken drugs that affect some enzymes called CYP3A4 (such as rifampin and St. John’s wort) in the past 7 days
- You are taking drugs that thin your blood such as aspirin and clopidogrel
- You have taken drugs that damp down your immune system (immunosuppressants) such as steroids in the past 2 weeks (unless this was either a cream or an inhaler)
- You have had severe side effects to
immunotherapy treatments  in the past
in the past - You are known to be sensitive to sorafenib, nivolumab (or any other monoclonal antibody) and anything it contains
- You have had a blood clot in the past 6 months
- You have a wound or a ulcer that is not healed or you have broken a bone in the past 3 months
- You have had severe bleeding in the past 8 weeks
- You have HIV
- You have hepatitis B, hepatitis C or hepatitis D
- You have an
infection  that needed treatment with antibiotics in the last 7 days
that needed treatment with antibiotics in the last 7 days - You have any other medical condition that the trial team thinks could affect you taking part in this study
- You are pregnant or breastfeeding
Trial design
This is an international phase 3 trial. The researchers need about 726 people worldwide and around 32 people in the UK to take part.
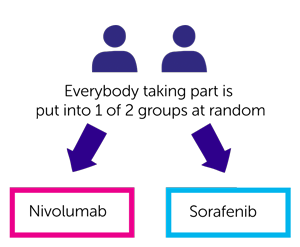
This trial is randomised. The people taking part are put into 1 of the following treatment groups by computer
- nivolumab
- sorafenib
Neither you nor your doctor will be able to decide which group you are.
Nivolumab
You have nivolumab as a drip into a vein every 2 weeks. It takes about 30 minutes.
You continue to have nivolumab for as long as the side effects aren’t too bad and the doctor feels it is helping you, even if your cancer gets worse.
Sorafenib
You have sorafenib as tablets. You take 2 tablets twice a day.
You continue taking sorafenib for as long as the side effects aren’t too bad and the doctor feels it is helping you, even if your cancer gets worse.
Quality of life
Everybody taking part of this trial will be asked to complete a quality of life questionnaire before starting treatment, at set times during the trial and then after you finish your treatment.
It will ask about how you have been feeling and what side affects you have had.
Blood tests
You have some extra blood tests as part of this trial. The researchers want to find out what happens to nivolumab in the body (you may hear these tests called  ).
).
They will also look for substances called  to see why treatment works better for some people than others.
to see why treatment works better for some people than others.
Tissue samples
You may also need to give a tissue sample (biopsy) of your cancer before you start treatment. This is to check if there is a marker on your cancer called PD-L1.
If you already had a tissue sample of your cancer taken either when you were diagnosed or during treatments, the trial team will ask to use a sample of it.
Hospital visits
You see a doctor and have some tests before taking part. These tests include:
- A physical examination
- Heart trace (
ECG  )
) - Heart ultrasound (
echocardiogram  )
) - CT scan or MRI scan
- Bone scan (if your doctor think is needed)
- Blood tests
- Urine test
After you start the treatment, you see the doctor for blood tests and a physical examination every 2 weeks.
You have a CT or an MRI scan
- every 8 weeks for the first 12 months
- every 12 weeks.
Your treatment continues for as long as your cancer stays the same or your doctor feels it is still helping you. If your cancer gets worse you stop treatment.
When you finish treatment you see the trial team after
- 1 month
- 3 months
After this the trial team will phone you every 3 months to see how you are.
Side effects
The trial team monitor you during the time you have treatment and you will be given a phone number to call them if you are worried about anything. The team will tell you about all the possible side effects before you start the trial.
The most common side effects of nivolumab are
- tiredness (fatigue)
- skin rashes
- diarrhoea
- tummy (abdomen) pain
- feeling or being sick
- loss of appetite
- a drop in the number of red blood cells (causing tiredness and breathlessness)
- high temperature (fever)
- joint pain or stiffness
We have information on sorafenib.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Daniel Palmer
Supported by
Bristol-Myers Squibb
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040



