A trial of a higher dose of radiotherapy for early rectal cancer (APHRODITE)
Please note - this trial is no longer recruiting patients. We hope to add results when they are available.
Cancer type:
Status:
Phase:
This is a trial comparing the standard dose of radiotherapy with a higher dose of radiotherapy for small cancers of the back passage (rectum). It is for people having radiotherapy or chemoradiotherapy who are not having surgery.
More about this trial
The usual treatment for people with small (early) cancers of the rectum is surgery. But some people aren’t able to have surgery. These people have either radiotherapy on its own or a combination of chemotherapy and radiotherapy (chemoradiotherapy).
Researchers think that a higher dose of radiotherapy might be better than the  . To find this out they need to compare people who have the standard dose of radiotherapy with people who have the higher dose.
. To find this out they need to compare people who have the standard dose of radiotherapy with people who have the higher dose.
In this trial some people will have either:
- chemoradiotherapy with radiotherapy using the standard dose or
- chemoradiotherapy with radiotherapy using the higher dose or
- radiotherapy on its own using the standard dose or
- radiotherapy on its own using the higher dose
The aims of this trial are to find out:
- how well the higher dose of radiotherapy works
- what the side effects are
- how it affects
quality of life 
Who can enter
The following bullet points list the entry conditions for this trial. Talk to your doctor or the trial team if you are unsure about any of these. They will be able to advise you.
Who can take part
You may be able to join this trial if all of the following apply. You:
- have adenocarcinoma of the back passage (rectum) confirmed by a sample of tissue (
biopsy  )
) - have cancer that is 5 cm or less at the widest part. Your doctor will know this.
- have had an
MRI scan  that shows the cancer
that shows the cancer - can have radiotherapy or chemoradiotherapy
- are not suitable to have surgery
- are up and about for at least half the day but might not be able to work (performance status 0, 1 or 2)
- have satisfactory blood test results
- are willing to use contraception during treatment and for 6 months after if you or your partner could become pregnant and you are to have chemoradiotherapy
- are at least 18 years old
Who can’t take part
You cannot join this trial if any of these apply. You:
- have cancer that is mostly of the mucinous type, have signet ring carcinoma or a neuroendocrine cancer
- have cancer that has spread to the
lymph nodes 
- have cancer that has grown through the muscle wall
- have cancer that has spread to another part of the body
- have had surgery to try and remove the cancer
- have had radiotherapy to the area between your hips (pelvis)
- have an opening from the bowel to the surface of the abdomen (colostomy or ileostomy) that has stopped working
- have had chemotherapy for bowel cancer
- have had another cancer apart from
non melanoma skin cancer  . You might be able to join if you had another cancer and there has not been any sign of it for the past 3 years
. You might be able to join if you had another cancer and there has not been any sign of it for the past 3 years - are pregnant or breastfeeding
Trial design
This is a phase 2 trial. The team need 104 people to join.
This is a randomised trial. You go into treatment groups. Neither you nor your doctor chooses which group you are in.
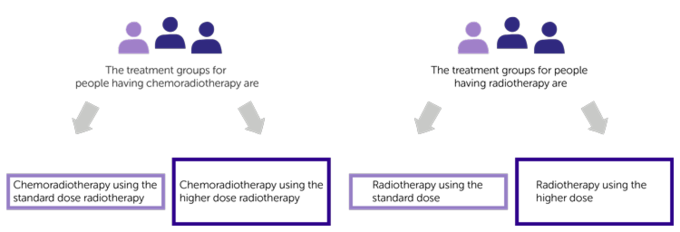
The treatment groups for people having chemoradiotherapy are:
- chemoradiotherapy using the standard dose radiotherapy
- chemoradiotherapy using the higher dose radiotherapy
The treatment groups for people having radiotherapy are:
- radiotherapy using the standard dose
- radiotherapy using the higher dose
Out of every 3 people who join the trial, 2 will have the higher dose of radiotherapy.
Before your radiotherapy you have a planning appointment. This is to work out where to give the radiotherapy.
You have  (IMRT). IMRT targets the cancer more precisely. This means the cancer gets a higher dose of radiotherapy and the surrounding healthy tissue gets a much lower dose of radiotherapy.
(IMRT). IMRT targets the cancer more precisely. This means the cancer gets a higher dose of radiotherapy and the surrounding healthy tissue gets a much lower dose of radiotherapy.
You have treatment Monday to Friday once a day for 5½ weeks (28 days).
People having chemoradiotherapy have either capecitabine or fluorouracil (5FU). Your doctor will talk to you about what is the best chemotherapy for you.
Capecitabine is a tablet. You take it twice a day on the days you have radiotherapy. You have a diary to write down how many tablets you take and when you take them.
You have 5FU as a drip into a vein. You have it once a day during the first 5 days of radiotherapy. You have it again during the last full week (days 21 to 25) of your radiotherapy.
Quality of life
You fill in 3 questionnaires:
- before starting treatment
- after finishing treatment
- and regularly during follow up
The questions ask about:
- your general health
- any symptoms or side effects you have
- your daily activities
This is a quality of life questionnaire.
Extra research
The team will ask to use the information from your radiotherapy and any scans you have along with the tissue sample from when you were diagnosed. They will use this to look at the  of the cancer cells to find out whether they can predict who might benefit from having the higher dose of chemoradiotherapy.
of the cancer cells to find out whether they can predict who might benefit from having the higher dose of chemoradiotherapy.
They might ask you to fill in a short questionnaire about people’s preference for cancer treatment.
You don’t have to agree to sharing your information or doing the questionnaire. You can still take part in the trial.
Hospital visits
You see the doctor for some tests before taking part. These tests include:
- a physical examination
- blood tests
- flexible sigmoidoscopy
- small piece of cancer tissue (biopsy)
- CT scan
- MRI scan
You see the doctor every week during treatment and at the end of treatment. This is for blood tests and to see how you are.
You will get a phone call from the team 2 weeks after treatment to see how you are.
After treatment you see the doctor at:
- 3 months
- 6 months
- 9 months
- 1 year
- 2 years
You have an MRI scan at:
- 3 months
- 6 months
You have a flexible sigmoidoscopy at:
- 3 months
- 6 months
- 1 year
Your doctor may decide that you should have additional scans or examinations. They will not be part of the trial.
Side effects
The trial team monitor you during treatment and afterwards. Contact your advice line or tell your doctor or nurse if any side effects are bad or not getting better.
Having the higher dose of radiotherapy might make the side effects worse.
Radiotherapy has early side effects and late side effects.
Early side effects can happen during radiotherapy and for a few weeks after. These include:
- diarrhoea
- pain and discomfort in the back passage (rectum) or anus
- problems passing urine such as difficulty passing urine, pain, not able to control when you pass urine
- loss of pubic hair which usually grows back
- tiredness (fatigue)
- irritation and inflammation of the vagina
Late side effects of radiotherapy can happen months or years after treatment. These include:
- bowel problems such as needing to go more often and urgently, difficulty passing poo, bleeding
- not being able to have children (infertility)
- early onset of menopause
- dryness and tightening of the vagina
- pain in the bones of the pelvis and occasionally breaking of the bones
- unable to have an erection (impotence)
- difficulty passing urine, needing to go urgently and blood in the urine
- change to skin colour and itching where you had treatment
We have information on:
- short term side effects of having radiotherapy
- long term side effects of having radiotherapy
- chemoradiotherapy
- capecitabine
- fluorouracil (5FU)
Your doctor or a member of the trial team will talk to you about the possible side effects of treatment before you agree to take part.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Simon Gollins
Dr Ane Appelt
Supported by
University of Leeds
Yorkshire Cancer Research
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040