A study comparing 2 operations for people with rectal cancer (HiP Study)
Cancer type:
Status:
Phase:
This study looked at 2 operations for people with rectal cancer and compared the side effects.
The study was for people who were due to have surgery to remove cancer in their rectum (back passage).
It was open for people to join between 2016 and 2019. The team published the results in 2020.
More about this trial
Surgery is the usual treatment for rectal cancer. The surgeon removes most of the rectum and attaches the bowel (colon) to the anus. They might create a pouch by folding back a small section of colon or by enlarging a section of the bowel (colon). This small pouch works like the rectum did before surgery. This is called a colo anal  .
.
This type of operation isn’t always possible. At the time of the trial people might have had one of the following instead:
- Hartmann’s procedure (HP)
- intersphincteric abdominoperineal excision (IAPE)
Both of these remove all the cancer in the rectum. With an IAPE the surgeon removes the anus as well.
These 2 operations are done equally by surgeons. When this study was done surgeons didn’t know which one worked best. So researchers ran this study to find out more.
The main aims of this study were to find out:
- how many people have either a HP or an IAPE operation
- what the side effects are
- how surgery affects quality of life
Summary of results
The researchers found the trial results support the use of either operation. They also found that the number of side effects was similar.
Study design
The type of surgery people had depended on what their surgeon thought best.
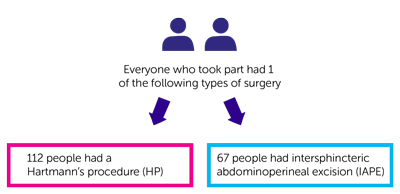
The team had the results for 179 people who took part in the study:
- 112 people had a Hartmann’s procedure (HP)
- 67 people had intersphincteric abdominoperineal excision (IAPE)
Results
After surgery the team looked at the number of problems (complications) and whether these were:
- related to having an operation (surgical) or
- medical, for example a heart problem
The team found the total number of complications were similar for both types of surgery. This was:
- 60 out of 112 people (54%) in the HP group
- 35 out of 67 people (52%) in the IAPE group
A similar number of people had side effects from surgery. This was:
- 48 out of 112 people (43%) in the HP group
- 32 out of 37 people (48%) in the IAPE group
A similar number of people also had medical problems after surgery. This was:
- 27 out of 112 (24%) in the HP group
- 17 out of 67 (25%) in the IAPE group
There was no difference in the care people had before and after surgery. The length of hospital stay was about the same for both groups.
Surgical side effects
12 people (11%) who had a Hartmann’s procedure developed an  in the area between the hip bones (pelvis). This was much more common if the surgeon could feel where the staples were put in to close the wound.
in the area between the hip bones (pelvis). This was much more common if the surgeon could feel where the staples were put in to close the wound.
People who had an IAPE operation had more problems with an infection in the area of the anus (perianal area).
Medical side effects
People who had IAPE had medical problems that were more severe than the other group. The researchers think this may have happened as the IAPE is a longer operation. They can’t be sure though.
The most common severe medical problems were:
- chest infections
- heartbeat changes
Quality of life
People filled in some questionnaires before surgery and afterwards. These asked about people’s health and how they were feeling. The team found no difference between the 2 groups in how people reported their health.
People who had the IAPE operation reported having a lower level of wellbeing than the other group at 90 days.
Conclusion
The study team concluded that these results support the ongoing use of either HP or IAPE in this group of people.
They say this should reassure surgeons that both procedures are acceptable and safe.
Where this information comes from
We have based this summary on information from the research team. The information they sent us has been reviewed by independent specialists ( ) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Mr Dale Vimalachandran
Supported by
Association of Coloproctology of Great Britain and Ireland
Bowel Disease Research Foundation
Countess of Chester Hospital
NIHR Clinical Research Network: Cancer
Northwest Surgical Trial Centre, Liverpool
Royal College of Surgeons of England
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040