Accelerator Award
We are currently unable to commit to funding future rounds of the Accelerator Awards. The co-funders (CRUK, AIRC and AECC) remain in active conversation about opportunities to support shared research priorities. We are continuing to support and monitor the current open awards.
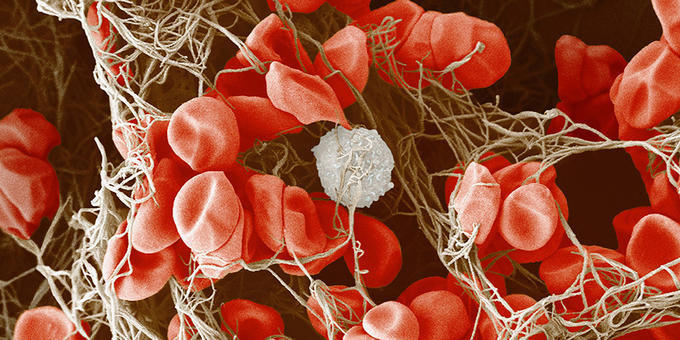
Scientific remit
The purpose of the Accelerator Award is to enable progress in translational cancer research through the development of tools, platforms and skills that form the foundations of such research. We fund ambitious programmes which typically have multiple strands. These may include:
- Producing datasets, tissue banks, cell lines or models
- Developing methods, protocols, software and standards
- Training, skills and knowledge sharing
Our partnership
Cancer is a global health issue, which is why we partnered with AIRC Foundation for Cancer Research and Fundación Científica de la Asociación Española Contra el Cáncer, the principal cancer research charities in Italy and Spain respectively. Our Accelerator Award is helping researchers share skills and resources for maximum patient benefit across borders.
Contact us
CRUK office
Brooke Lumicisi
Tel: 0203 469 5155
AIRC office
Luana Grimolizzi
AECC office
Marta Puyol
 Accelerator Award
Accelerator Award