

TET focuses on the ‘implementation gap’ - the inconsistent adoption of proven interventions - by gathering evidence to address barriers to adoption.

Diagnosis information for primary care clinicians, including guidelines and supportive documentation.
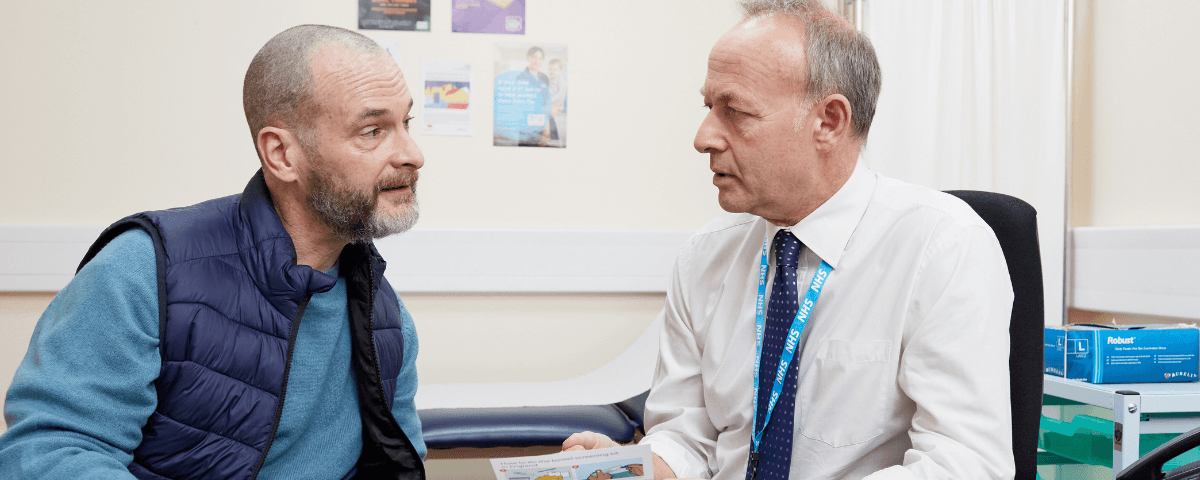
A selection of tests/investigations that a health professional may use before considering the need for referral.

Public and voluntary sector partnerships to support and drive forward work on early diagnosis of cancer (formerly NAEDI).
A unique early diagnosis initiative exploring alternative approaches to cancer diagnosis and care pathways.

ICBP produces research to help identify best international practice and generate insights needed for policy and practice change.
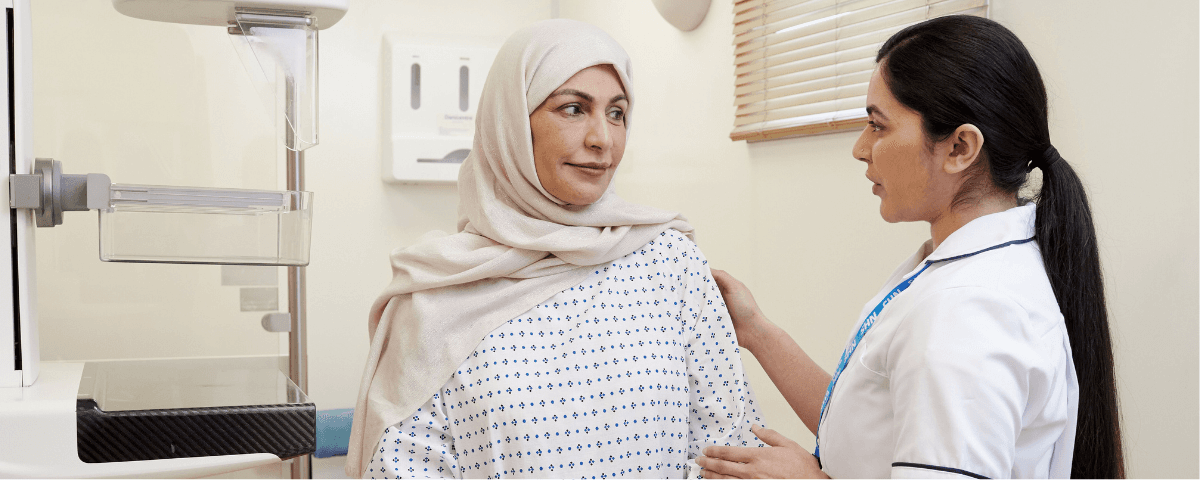
Diagnosing cancer early must remain a priority in the health service. We work to ensure that diagnosing cancer early stays at the top of the agenda.
This app gives clinicians quick and easy access to calculators and guidelines for investigating and managing pulmonary nodules. For iOS
Tools and information to allow investigation of cancer diagnosis through primary care.
Explore a selection of reports and publications from the experts at Cancer Research UK, and through various collaborations.
Topics include: summaries of the state of cancer, projections, risk factors and preventability, symptom awareness investigation, intervention success, barrier identification, treatments received and more.
Newsletters targeted at health professionals which provide intelligence to support evidence-based decision making and updates on our activities, as well as our bespoke GP newsletter which includes best practice guidance, practical tools and expert resources.
See the range and sign upYou are welcome to reuse this Cancer Research UK content for your own work. Credit us as authors by referencing Cancer Research UK as the primary source. Suggested styles are:
Web content: Cancer Research UK, full URL of the page, Accessed [month] [year].
Publications: Cancer Research UK ([year of publication]), Name of publication, Cancer Research UK.
Graphics (when reused unaltered): Credit: Cancer Research UK.
Graphics (when recreated with differences): Based on a graphic created by Cancer Research UK.
When Cancer Research UK material is used for commercial reasons, we encourage a donation to our life-saving research. Send a cheque payable to Cancer Research UK to: Cancer Research UK, 2 Redman Place, London, E20 1JQ.
Donate online