Our work has revolutionised what we know about cancer and how we can beat it.
Our research strategy builds on what's already been achieved and sets out how we'll work with our world-class research community towards a better future.
Read our research strategyOur strategy puts discovery research and excellence at the heart of what we'll do to understand the mechanisms of how cancer develops and progresses.
It's built around four objectives – to discover, detect, prevent, and treat – so that progress in understanding the fundamental biology of cancer leads to new prevention measures, tests and treatments.
To achieve this, we will spend £1.5bn between 2022 and 2027, investing in creative people and transformational research. We will support research to reduce cancer inequalities and improve outcomes for everyone. And we’ll involve people affected by cancer in our work.
Explore our commitment to patient and public involvement
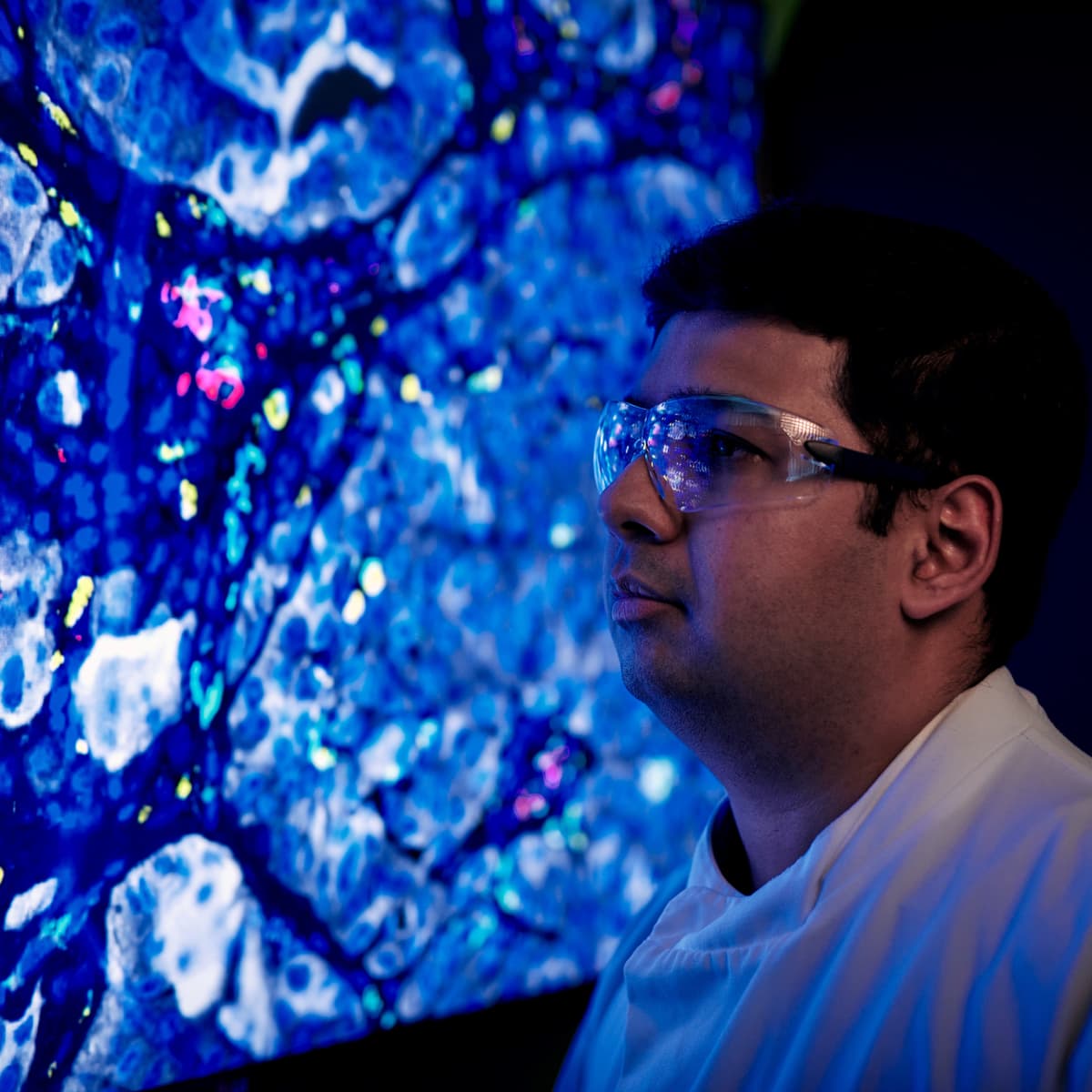
Our discovery research portfolio provides fundamental insight into the mechanisms by which cancer develops, progresses and responds to treatment.
We’re advancing transformative cancer outcomes through research focussed on early detection of cancer and pre-cancerous changes, underlying biology of cancers, cancer emergence and progression.

We support a wide range of prevention and population research aimed at understanding the epidemiology of cancer, cancer risk, incidence and survival and preventative interventions.

Our robust portfolio of clinical studies spans the clinical pipeline, including early phase and first-in-human trials, ambitious and innovative trial design, and clinical infrastructure.
We aim to leverage the enormous potential of data science and advanced analytics by creating a research culture and community supporting timely, transparent and ethical curation and use of data in cancer research.

We’re building strong, sustainable research communities in notoriously hard-to-treat cancers such as brain, lung, oesophagus, pancreas, liver and stomach, and can support you as you move into this field.

We’re prioritising research in children's and young people's cancers to address the unique barriers researchers and partners face in driving progress in this area.
We're committed to driving therapeutic innovation in oncology through our translational arm, Cancer Research Horizons. We have expertise and capabilities to translate early concepts to patient benefit, encompassing deep cancer biology knowledge and extensive drug discovery experience.
Our strategy renews our focus on making discoveries, driving progress, bringing hope - leading us to a world where everybody can lead longer, better lives, free from the fear of cancer.
In 2014 we outlined our approach to accelerate progress in priority areas including early detection, translation, and developing world-class cancer researchers.
We have a range of opportunities, suitable for wherever you are in your career, whether you're new to the lab or growing your research group.