Infections (e.g. HPV) and cancer
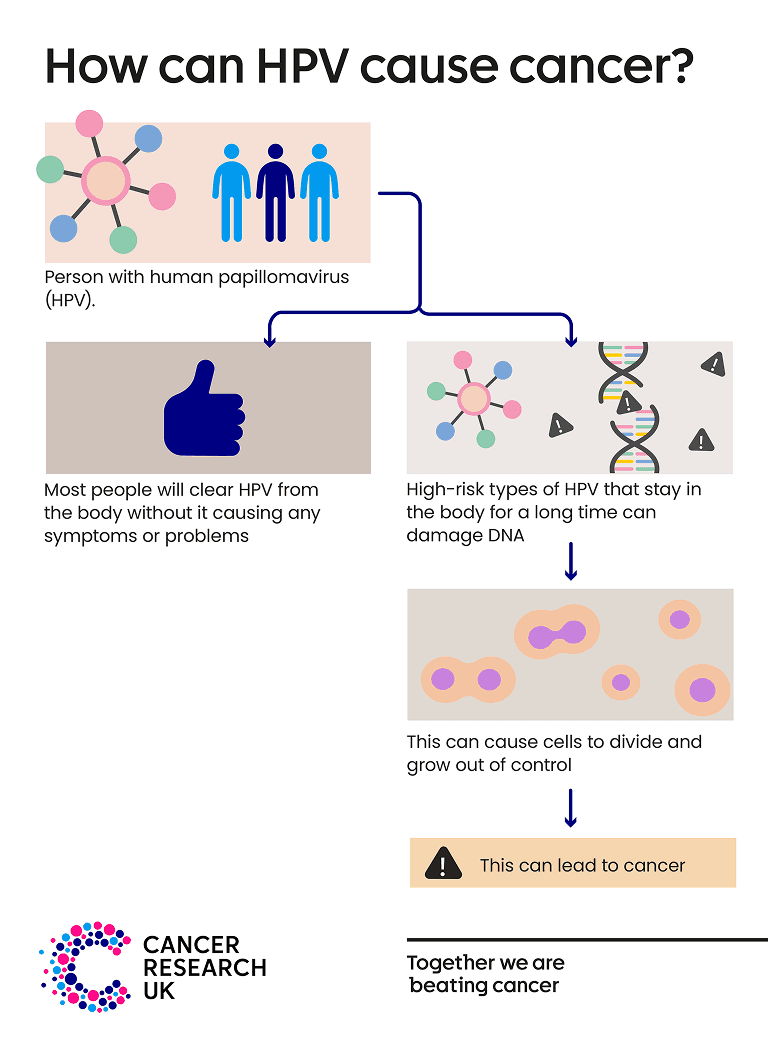
The human papillomavirus (HPV) is a common virus that infects the skin and cells lining the inside of the body, including the mouth, throat, and genitals. HPV infection usually causes no symptoms. For most people, HPV will be cleared from the body and they will never know they had it.
HPV usually spreads through close skin-to-skin contact. This is usually during sexual activity, including vaginal, anal, or oral sex.
Yes, there are hundreds of different types of HPV. Some types are called ‘low risk’ HPV. These types can cause problems such as genital warts, or warts and verrucas on the hands and feet.
There are around 14 ‘high-risk’ types of HPV that increase the risk of some types of cancer. People infected with high-risk HPV for a long time are more likely to develop cancer.
But remember, most HPV infections are cleared from the body and do not cause any symptoms or problems. And having high-risk HPV doesn’t mean that someone will definitely get cancer.
This page focuses on high-risk types of HPV, as these types can cause cancer.
Cervical cancer is the main type of cancer linked to HPV. Nearly all cases of cervical cancer are caused by HPV. HPV can also increase the risk of some types of head and neck cancer, including oropharyngeal cancer (a type of throat cancer) and mouth cancer. Around 70% of these cancers are linked to HPV.
Most cancers of the vagina, vulva, penis, and anus are caused by HPV. But these cancer types are uncommon.
Most of the time the body clears HPV without it causing any problems. But high-risk HPV types can cause cancer if they stay in the body for a long time.
If this happens, the HPV virus can change the DNA inside our cells and cause them to behave differently. Over time, the affected cells can grow out of control and lead to cancer. This can take many years.
HPV is very a common infection, and most people will get HPV at some point in their lives. There are some ways to help protect yourself from HPV and reduce the risk of cancers caused by HPV.
The HPV vaccine helps to prevent cancer by protecting against HPV.
All children aged 11-13 in the UK can get the HPV vaccine. It’s also available for free to people up to the age of 25 who missed their vaccine when they were offered it, men who have sex with men (up to the age of 45), and some transgender people (up to the age of 45).
Find out more about HPV vaccination.
Cervical screening aims to prevent cervical cancer. It tests for high-risk HPV and looks for early cell changes caused by HPV. These cells can then be monitored or treated before they have a chance to become cancerous. Cervical screening in the UK is offered to most women, some trans men, and some non-binary people, who are aged 25-64.
Screening is for people who don’t have symptoms. If you notice anything that isn’t normal for you, don’t wait for your next screening appointment, talk to your doctor.
Find out more about cervical screening.
Smoking makes it harder for the immune system to protect against HPV infections and to clear HPV from the body. Not smoking lowers the risk of HPV and cervical cancer.
Find out more about how to stop smokingUsing a condom or dental dam during sex, including oral sex, makes getting or passing on HPV less likely. This is true no matter your gender or that of your partner.
As these don’t cover the whole genital area, they do not provide complete protection from HPV but can help reduce the risk. .
Last reviewed: 24 Jan 2024
Next review due: 24 Jan 2027
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.