Last reviewed: 29 January 2025
Last reviewed: 29 January 2025
Bowel cancer screening can support cancer prevention and drive earlier diagnosis. Be Clear on Cancer (BCOC) campaigns were carried out to drive bowel screening uptake in England and Wales to support the national screening programmes.
This campaign was the first to focus on cancer screening, as previous BCOC campaigns were focused on raising awareness and help-seeking for cancer symptoms. Pilot campaigns were run by Cancer Research UK to assess the impact of a screening focused campaign.
Endorsement flyers with gloves and a poo catcher were sent to people eligible for bowel cancer screening as part of a pilot in London in 2014. Uptake increased by 6.1 percentage points among 60-69 year olds and by 7.3 percentage points among 70-74 year olds. In 2015, a Welsh pilot assessed sending an endorsement letter to first time invitees and a pack with gloves to non-responders from deprived areas. Results show uptake increased by 9.1 percentage points among first timers and 3.2 percentage points among more deprived non-responders.
In 2017, BCOC campaign activity was carried out across the North West of England to raise awareness and uptake in the eligible population for bowel cancer screening. This area was selected using local uptake statistics at the time showing uptake in the North West of England was as low as 40%, compared to 58% nationally
. In 2018, we supported Public Health Wales to launch a BCOC bowel cancer screening campaign to encourage more people aged 60-74 to participate in bowel cancer screening. At the time, bowel screening uptake was below the acceptable target of 60% in Wales and much lower in more deprived areas .The campaigns were aimed at 55-74 year olds from lower socioeconomic groups, with a focus on men. This focus was chosen as we know that men from deprived areas are least likely to participate in bowel cancer screening. The target age group ensured the campaign reached both those currently eligible and those soon to be eligible for screening.
An advertising campaign including TV, posters at bus stops, adverts in newspapers and on Facebook ran for 12 weeks.
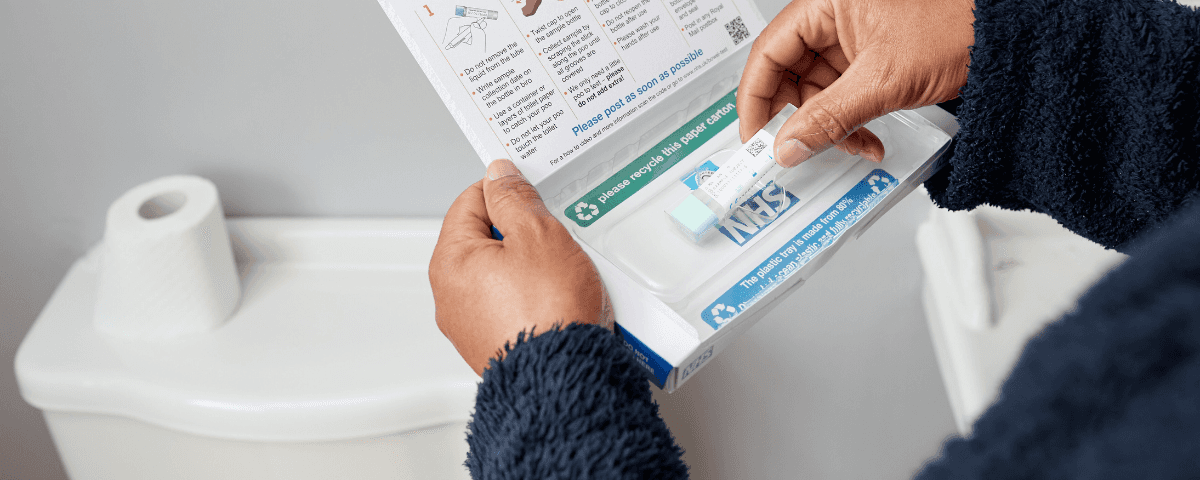
In England, two versions of a direct mail were sent out 2-3 days after the NHS bowel screening kit. The first was a Cancer Research UK endorsement letter sent to first time invitees to bowel screening. The second version was a Cancer Research UK endorsement pack with latex free gloves sent to bowel screening non-responders. People who’d been screened in the past were not targeted with direct mailing.
The key message for the public was ‘This little kit could save your life’.
Other key messages included:
If you're aged 60-74 you'll be sent a free bowel cancer screening kit in the post, once every two years.
It's meant for people with no symptoms.
It can help detect bowel cancer early, when it's easier to treat successfully.
So don't ignore it, take the test.
Be Clear on Cancer.
The change in bowel screening uptake was analysed across a range of metrics including screening history, age, gender and deprivation. Comparison of people invited before the campaign and with areas not exposed to advertising during the campaign was performed.
Cancer outcomes data were analysed to understand the number of pre-cancerous adenomas/polyps and cancer detected through screening.
The impact of the campaign on services was assessed by checking:
number and waiting times for specialist appointments and colonoscopies
62-day wait times from urgent referrals to treatment starting
screening centre data on demand pre, during and post campaign
questionnaire for people attending specialist or colonoscopy appointments
GP attendance data
Be Clear on Cancer was a cancer awareness campaign led by Public Health England, working in partnership with the Department of Health and NHS England. This page contains links to documents that we hope you find useful. Please note however that the views or opinions expressed within those links are not necessarily those of Cancer Research UK.
Office for Health Improvement and Disparities. Fingertips.
Public Health Wales. Annual statistical reports.