Last reviewed: 15 October 2025
Last reviewed: 15 October 2025
Bowel cancer is the fourth most common cancer in the UK, with around 46,600 new cases every year (2018-19, 2021). Patients who are diagnosed with bowel cancer at its earliest stage have more treatment options available that are more likely to be successful compared to patients diagnosed at a late stage.
Bowel cancer screening reduces deaths from bowel cancer
. It aims to both prevent bowel cancer through the identification and removal of pre-cancerous polyps or adenomas , and to detect it at an early stage before symptoms have a chance to develop. There are separate bowel cancer screening programmes for each UK nation, with differences between them. These are outlined in the table below and in our bowel cancer screening at a glance resource. (PDF, 160 KB)Bowel | England | Scotland | Wales | Northern Ireland |
|---|---|---|---|---|
Age | 50-74 | 50-74 | 50-74 | 60-74 |
Frequency | 2 yearly On request from age 75 | 2 yearly On request from age 75 | 2 yearly | 2 yearly |
Test | Faecal Immunochemical Test (FIT) | |||
Threshold | 120 µg/g [a] | 80 µg/g | 80 µg/g | 120 µg/g |
Uptake [b] | 68% (2023 - 24) | 66% (2022 - 24) | 66% (2023 - 24) | 67% (2023 - 24) |
[a] NHS England is beginning to reduce the FIT threshold to 80 µg/g across several early-adopter sites.
[b] Caution should be taken when making comparisons across countries due to differences in time periods of data, changes to age ranges and/or differences in the definitions of coverage and uptake of screening.
For practical support, our bowel cancer screening primary care good practice guide offers tools and resources to help primary care teams support informed participation.
Download our bowel cancer screening good practice guide. (PDF, 1.1 MB)
Find information on eligibility, the test used FIT, uptake data, promoting informed choice, safety netting and surveillance.

Discover who’s less likely to participate in bowel cancer screening, the barriers people face, and how targeted interventions can help address inequalities in uptake.

Explore the opportunities to optimise bowel screening – including age expansion, enhanced FIT sensitivity and risk stratification.
Download our bowel cancer screening primary care good practice guide(PDF, 1.1 MB) for practical steps practices across the UK can take to support informed participation in their local population.
Explore our bowel cancer screening hub developed with Doctors.net UK for educational content (login required).
Visit our cancer early diagnosis data hub for the latest UK statistics on bowel cancer incidence, survival by stage, and screening uptake.
Visit our FIT symptomatic webpages for an overview of the key differences between the use of FIT for screening vs. for investigating people with symptoms across the UK nations.
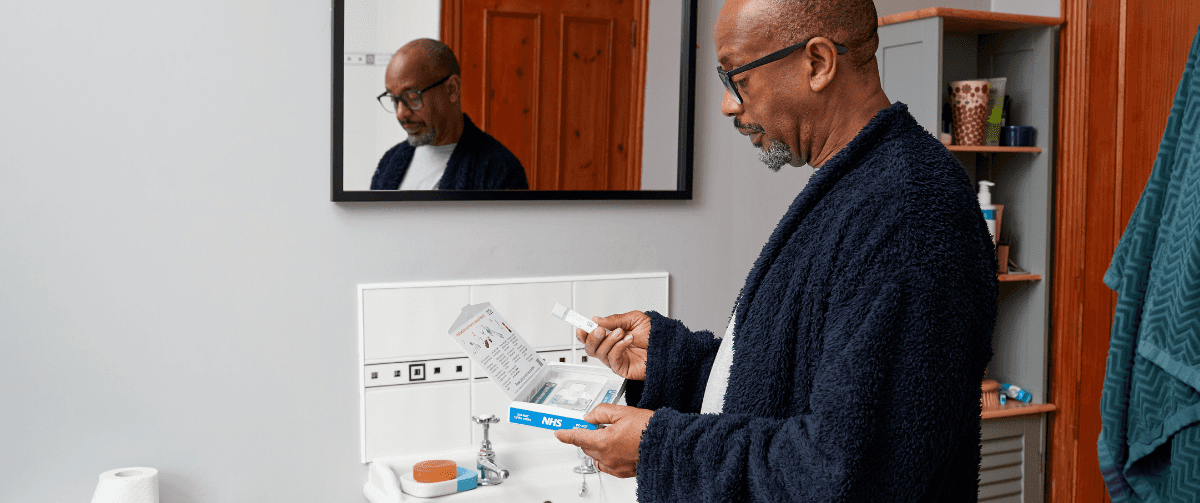
Our public-facing bowel cancer screening webpages provide accessible information on bowel cancer screening, including the benefits and harms, eligibility criteria, and instructions on how to complete the test.
An animated video that explains how to complete the bowel cancer screening test kit. There's a subtitled version too.
‘How to do the bowel cancer screening test’ - subtitled version
‘How to do your bowel screening test’ (Wales) - English language
‘How to do your bowel screening test’ (Wales) - Welsh language
Step-by-step infographics on how to complete the bowel cancer screening test kit and practical tips on how to collect the poo sample.
England(PDF)
Scotland(PDF)
Northern Ireland(PDF)
Each UK nation has its own hub of resources to support people to take part in bowel cancer screening, with nation-specific information in multiple languages and accessible formats:
Scholefield JH, Moss SM, Mangham CM, et al. Nottingham trial of faecal occult blood testing for colorectal cancer: a 20-year follow-up.Gut 2012;61:1036-1040.
Granger, SP, Preece, RAD, Thomas, MG, Dixon, SW, Chambers, AC, Messenger, DE. Colorectal cancer incidence trends by tumour location among adults of screening-age in England: a population-based study. Colorectal Dis. 2023; 00: 1–12.
Stay up-to-date with the latest cancer research information.