External radiotherapy for thyroid cancer
External radiotherapy uses a radiotherapy machine to aim radiation beams at a cancer. This destroys the cancer cells.
It is important that the treatment dose and where you need to have the radiotherapy is worked out carefully before treatment starts. You have an appointment for your radiotherapy team to plan this.
Your appointment takes from 15 minutes to 2 hours.
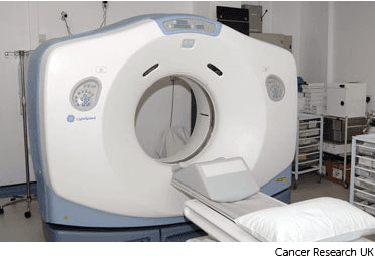
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
Your radiographers tell you what is going to happen. They help you into position on the scan couch. You might have a type of firm cushion called a vacbag to help you keep still.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You need to lie very still. Tell your radiographers if you aren't comfortable.
You might need an injection of contrast into a vein in your hand. This is a dye that helps body tissues show up more clearly on the scan.
Before you have the contrast, your radiographer asks you about any medical conditions or allergies. Some people are allergic to the contrast.
Once you are in position your radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. Your radiographers can see and hear you from the CT control area where they operate the scanner.
You lie on the scanner couch with the treatment area exposed.
Watch our video about radiotherapy planning. It is just under 3 minutes long.
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
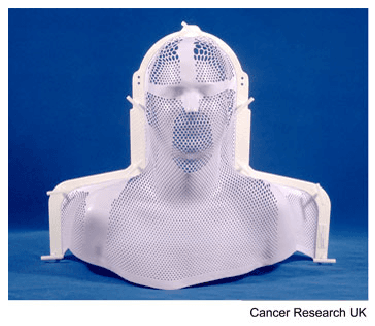
Your treatment team might make a mask for you if you are having radiotherapy to your head and neck area. They are also called radiotherapy shells.
Your treatment team will make one for you to wear during your treatment sessions. It will help you to keep very still when you have radiotherapy.
The radiographers make marks on the mask and use the marks to line up the radiotherapy machine for each treatment.
The process of making the shell can vary slightly between hospitals. It usually takes around 30 minutes.
You need to wear clothes that you can easily take off from your neck and chest. You also need to take off any jewellery from that area.
Facial hair, long hair or dreadlocks can make it difficult to mould the shell. The radiotherapy staff will tell you if you need to shave or to tie your hair back.
A technician uses a special kind of plastic that they heat in warm water. This makes it soft and pliable. They put the plastic on to your face, neck and chest so that it moulds exactly.
After a few minutes the plastic gets hard. The technician takes the mask off and it is ready to use.
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.
Go to information about having external radiotherapy for thyroid cancer
Last reviewed: 07 Sept 2023
Next review due: 07 Sept 2026
You have external radiotherapy in the hospital radiotherapy department as a course of treatment. You usually go to the hospital for treatment on week days.
Radiotherapy means the use of radiation, to treat cancer cells. You might have internal radiotherapy (radioactive iodine) or external radiotherapy for thyroid cancer.
Possible treatments include surgery, radiotherapy, targeted drugs and chemotherapy. What treatment you have depends on your type and stage of thyroid cancer.
Practical and emotional support is available to help you cope with thyroid cancer.
Thyroid cancer is when abnormal cells in the thyroid gland start to divide and grow in an uncontrolled way.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.