Brain tumours
Your child will need a number of tests if their doctor suspects they have a brain tumour. The tests they might have include one or more of the following:
a neurological examination which tests your child’s nervous system
an MRI scan
a CT scan
blood tests to check your child’s general health and tumour marker levels
taking a sample of tissue (biopsy)
tests on the tumour to check for changes in genes (biomarkers)
a spinal fluid test (lumbar puncture)
These tests aren’t generally painful but your child will have to keep still while having them. To help keep them still for some tests, your child might need to be drowsy () or asleep ().
The team caring for your child are used to helping children have these tests. They will go through everything with you. They will also do everything they can to prepare them and you for the tests.
The following is more information about each individual test and what to expect.
Testing your nervous system is called a neurological examination. Your child’s doctor might:
test your child’s muscle strength by getting them to squeeze the doctor's hands or push against the doctor’s hands with their feet
look to see if they have any numbness anywhere in their body
tap their knee with a small rubber hammer to check their reflexes
look into the back of your child’s eyes to see if there are any changes
see how your child follows commands – they might see how well they are reading or writing if your child is able
There is usually no preparation for these tests.
Your child can usually eat, drink and play normally after having a neurological examination.
MRI stands for magnetic resonance imaging. An MRI scan creates pictures using magnetism and radio waves. MRI scans produce pictures from angles all around the body and shows up soft tissues very clearly.
Your child usually has an MRI scan to help:
diagnose a brain tumour
find out where it is
find out if it has spread
monitor how treatment is working
In some cases MRI scans are done during surgery to see if all the tumour has been removed.
Some children might have specialised MRI scans depending on the type of surgery they are having. Some of these include:
magnetic resonance spectroscopy (MRS) scans which looks at the chemicals in the tumour
perfusion MRI scans that look at the blood flow in different parts of the brain
diffusion weight MRI scans (DWI or DW-MRI) which measure the movement of water molecules in cells. This can show differences between fast and slow growing cells.
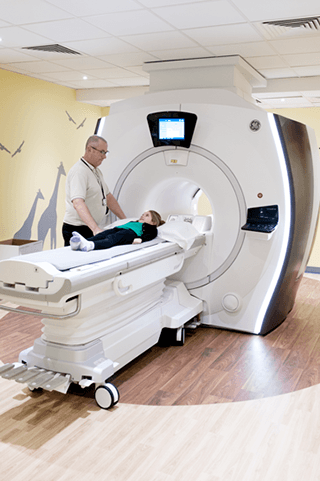
Many young children have a sedative or general anaesthetic to help them lie still on the couch for the scan. For most MRI scans, they need to lie still for around 30 minutes. Your child usually has an injection of a special dye before or during the scan to help make the pictures clearer.
Your child stays on the day unit or children's ward for a couple of hours after the scan. This is so the team can be sure they have recovered and are awake enough from the sedation or general anaesthetic.
The nurses on the unit usually check that your child has had:
something to drink
something to eat or has drunk some milk
a wee
This can help the nurses see if your child has recovered from the sedative drugs.
CT stands for computed tomography. A CT scan uses x-rays and a computer to create detailed pictures of the inside of your body. It takes pictures of the body from different angles. A computer then puts them together to give a series of pictures. It can help doctors find out if there is a tumour and where it is. It can’t show exactly what type of tumour it is.
The scan itself is painless. Your child's specialist team will let you know how:
to help your child prepare
long your child needs to not eat or drink before their sedation
long the scan is likely to be
The may give your child an injection of a type of dye (contrast medium). They give this through a small thin tube (a cannula) in their hand or arm.
Some young children have a medicine to make them feel sleepy and relaxed (sedative). Or they may need a general anaesthetic to help them lie still on the couch for the scan. Other children can have the scan awake with your support and help from the specialist team.
The couch slowly slides backwards and forwards through the hole of the scanner. The machine takes pictures as it moves.
Your child stays on the day unit or the children's ward for a couple of hours after the scan. This is so the team can be sure they have recovered and are awake enough from the sedation or general anaesthetic.
The nurses on the unit usually check that your child has had:
something to drink
something to eat or has drunk some milk
a wee
This can help the nurses see if your child has recovered from the sedative drugs.
Your doctor might suggest you give your baby a feed as normal and then wrap them in a soft towel or blanket. This can help your baby lie still for their CT or MRI scan.
Babies that have had a feed and wrap scan don't need the same level of monitoring after. This is because they haven't had any medicine to make them feel sleepy.
Blood tests can check:
your child’s general health, including how well their liver and kidneys are working
the numbers of blood cells - this is often called a blood count, or full blood count
If your child’s doctor thinks they might have a secreting germ cell tumour, they’ll have blood tests to check for certain hormone levels. These are known as tumour markers. Tumour markers are substances that either the tumour or your body produces as a response to a cancer. They’re found in the blood, tissue in the body or body fluids such as urine.
The following are examples of tumour markers doctors look for with secreting germ cell tumours:
alpha fetoprotein (AFP)
beta human choriogonadotropin (beta HCG)
A doctor, nurse or a takes a small amount of blood from your child. This is usually from the back of the hand, the inside of the elbow or wrist area.
Most blood tests take a couple of minutes.
The specially trained staff will help your child feel as comfortable as possible. Things that can make it easier for your child include:
They might use a local anaesthetic. This means that they apply a numbing spray or cream to your child's skin before they do the test. This should mean it’s less painful for your child, although they might still feel the needle go in.
Distraction could be singing, counting, watching something on your mobile phone or a DVD.
Holding your child while they are having their blood test can make them feel safe and secure. You can give them a cuddle afterwards if you’re unable to hold them during their test.
Your child can usually eat, drink and play as normal after a blood test.
Your child’s doctor might want to take a sample of the tumour (biopsy) seen on a scan. A pathologist looks at the cells down a microscope to find out exactly what type of brain tumour it is. This is so they can be sure what treatment is best.
Not every child has a biopsy. It might be safer for them to have surgery to remove the tumour straight away. Or the tumour might be in an area of the brain that’s difficult to biopsy. This means the doctors find out the type of brain tumour after surgery.
Your child has a general anaesthetic for this test. This means they are asleep and can’t feel anything during the test.
Your child’s surgeon carefully drills a small hole in your child’s skull. They put a needle into the hole and remove a small piece of the brain tumour. This might sound quite frightening. But the team consider the benefits and the risks of the procedure before suggesting a biopsy.
A specialist surgeon known as a paediatric neurosurgeon does the brain surgical biopsy. There are different types of surgical biopsy. The difference between them is the way the surgeon does the biopsy.
Your child usually stays on the children’s ward for a night after the biopsy. This is so the team can be sure that they are awake enough from the anaesthetic. The nurses on the unit usually check that your child has had:
something to drink
something to eat or drunk some milk
a wee
The nurse will also make sure your child has a clean and dry dressing over the site of the test.
A biopsy is a safe test. Your child’s doctor goes through the risks and benefits with you. The most common risks are bleeding from the site or infection. Your team gives you a telephone number to call if you have any problems at home. If in doubt, give them a call.
Your doctor may arrange tests to look for changes in the sample of your child’s brain tumour. They call these changes .
This can help them:
get more information about the type of brain tumour
work out how quickly the brain tumour might grow
work out how likely the brain tumour will respond to treatment
A lumbar puncture is a test to check the fluid that circulates round the brain and spinal cord. This is called cerebrospinal fluid or CSF. A lumbar puncture can check for cancer cells or for infection in the CSF. Using a needle, your child’s doctor or specialist nurse, takes a sample of the CSF from their lower back.
Children who have cancerous (malignant) brain tumours usually have this test. It usually happens 2 weeks after the operation to remove the brain tumour.

Most children have a general anaesthetic for this test. But occasionally some older children might be able to have a local anaesthetic.
The area where the needle goes in is numbed with a local anaesthetic. If your child has this test under local anaesthetic they might still feel some pressure and a slight soreness when the needle goes in.
When the area is numb, the doctor or nurse puts the lumbar puncture needle in through the skin. It goes into the small of the back and into the space around the spinal cord.
Once it's in the right place, the fluid drips out into a pot. This only takes a few seconds. The doctor or nurse takes the needle out and puts a dressing or plaster on your child’s back.
Your child’s team will talk you through the benefits and risks of having a lumbar puncture. There is a risk of bleeding and infection, but this is very rare.
You should contact your hospital if your child is at home after a lumbar puncture and they get symptoms such as:
a severe headache
being sick
their eyes are sensitive to bright light
tingling or numbness in their legs
Your nurse will tell you what symptoms to look out for and who to contact if you have any problems at home.
It’s likely your child can go home the same day, unless they are staying in hospital for other tests.
Find out about the different types of brain tumours in children
Last reviewed: 13 Dec 2022
Next review due: 13 Dec 2025
Tumours affecting the brain and central nervous system are the second most common type of children’s cancer in the UK. Around 420 children are diagnosed with these tumours each year in the UK.
Brain tumour symptoms can be very similar to those of childhood illnesses. Take your child to the GP if they have any symptoms of a brain tumour.
The main treatments for children’s brain and spinal cord tumours are surgery, radiotherapy and chemotherapy.
We don't know what causes or how to prevent most childhood cancers. There are some factors that can increase the risk of cancer in children.
It is essential that parents and other close family have support. Find out what is availble and who can help.
Brain tumours are the second most common type of children’s cancer in the UK. Around 420 children are diagnosed with these tumours each year in the UK.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.