Treatment for lung cancer
The 2 types of thermal ablation for lung cancer are:
radiofrequency ablation (RFA)
microwave ablation (MWA)
Radiofrequency ablation (RFA) is a type of electrical energy.
You have RFA using one or more special needles called needle electrodes. The electrical current from the needle heats the cancer cells to high temperatures, which destroy them. The heat only travels a short distance, so it doesn’t generally affect the rest of your lung tissue. You usually have the needles through your skin into the tumour. This is called percutaneous ablation.
You have microwave ablation (MWA) in a similar way to RFA. But MWA uses a different type of energy called microwave energy.
Your doctor might recommend RFA or MWA if you have:
an early stage lung cancer and you can't have surgery, or you don't want surgery
a small number of secondary cancers (metastases)
a large lung cancer that can’t be removed with surgery, such as one that is blocking your airway and making it hard to breathe
pain from a cancer that has grown into the chest wall
You can have treatment several times. You might have RFA or MWA alone or with other treatments.
You have an appointment at the pre assessment clinic about a week before your treatment. This is to prepare you for the treatment and check you are well enough to have it.
You might need blood tests to check how well your liver and kidneys are working and whether your blood clots normally.
The nurse explains exactly what will happen on the day. Do use this time to ask any questions you might have.
Let them know if you have any allergies or are taking any medicines that change how your blood clots. These medicines include:
blood thinning medicines such as warfarin, rivaroxaban and dabigatran
Your doctor might ask you to stop the above medicines for some time before you have thermal ablation.
You go into hospital on the day of your treatment or the evening before.
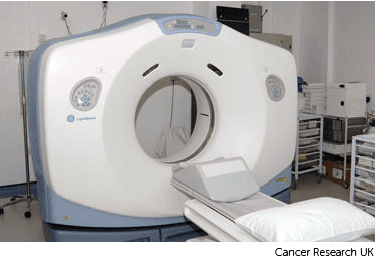
You have the treatment in the operating theatre or scanning (x-ray) department of the hospital.
You may be asked not to eat or drink anything after midnight before your procedure. Your doctor will tell you which medication you may take in the morning. Your appointment letter will also give you more information.
You might have RFA or MWA under general anaesthetic, which means you are asleep. Or you might have a drug that makes you sleepy (sedation) and a local anaesthetic to numb the skin above the lung. You will also have strong painkillers during treatment.
Your doctor (interventional radiologist) uses either an ultrasound scan or a CT scan to guide the needle through your skin into the tumour. The needle heats the tumour and destroys it. The time this takes varies. Each thermal ablation treatment takes about 10 to 30 minutes. If your doctor has to do several ablations, it may take longer. The entire procedure usually takes about 1 to 3 hours.
Nurses monitor you throughout the procedure. They check your blood pressure, pulse and oxygen levels.
Your doctor removes the needle when the treatment has finished and covers the area with a dressing.
You have a chest x-ray after the procedure. This is to ensure the lung has not collapsed during the procedure (pneumothorax).
You usually have to stay in bed for a few hours after the procedure. You can start eating and drinking once you are fully awake and feel up to it. You usually go home the next day. You should be back to doing your normal activities after about a week.
You usually have a scan about 4 weeks afterwards to check how well the treatment has worked.
As with any medical procedure there are possible side effects or complications. Your doctor makes sure the benefit of the treatment outweighs these risks. Side effects include:
You will probably have some discomfort or mild pain where the needle has gone into your skin.
You will have painkillers to take home, although you may not need to use these. Contact your healthcare team if you are taking painkillers and they are not working. Also, let them know if you still have pain 1 or 2 weeks later or if the pain is getting worse.
Some people have flu-like symptoms that start about 3 days after treatment and can last up to a week. You feel generally unwell, have body aches, and you may feel sick. This is due to a side effect called post ablation syndrome.
Before you go home, your healthcare team will explain this syndrome. They will go through what medicines you can take to relieve your symptoms.
Contact your healthcare team if your symptoms don’t improve, or your temperature is above 37.5C.
There is a small risk of infections such as:
a skin infection where the needle has entered the skin
a lung infection
Contact your healthcare team if you have a temperature above 37.5°C or notice any signs of a skin infection around the needle's insertion area. This may include:
swelling
redness
liquid such as puss coming out
This happens when air leaks into the space between the lung and the chest wall. If the lung has collapsed, you might have a small tube into the area to remove the air pocket. The tube is called a chest drain. The tube stays in place for a few days.
There is a small risk of damage to some of the nerves supplying the arm. This is usually if the site of the lung cancer is close to the armpit. Damage may cause loss of sensation or loss of some strength. It usually resolves by itself but can be permanent in some people.
Another risk is bleeding caused by the needle going into the lung. This is uncommon. Your doctor and nurses monitor you closely during and after treatment. So, if this happens, they deal with it straight away.
Last reviewed: 16 Oct 2025
Next review due: 16 Oct 2028
Lung cancer starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Cancer that starts in the lung is called primary lung cancer.
Lung cancer starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Cancer that starts in the lung is called primary lung cancer.
Your treatment depends on several factors. These include what type of lung cancer you have, how big it is and whether it has spread (the stage). It also depends on your general health.
There is support available during and after treatment to help you cope. This includes support from your clinical nurse specialist, cancer charities, community services, and family and friends.
Feeling short of breath can be hard to live with. It can make you feel tired and like everything is a struggle. But some things can help you to cope.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.