Hair loss and cancer treatment
Hair loss is one of the most well known side effects of cancer treatment. For many people losing their hair can be distressing and devastating. It can be a constant reminder of your cancer and what you’re going through. But for most people, their hair will grow back once treatment has finished.
Whether you lose your hair depends on:
the type of drug or combination of drugs you're having
the amount (dose)
your individual sensitivity to the drug
your drug treatment in the past
Chemotherapy is the type of cancer treatment most likely to cause hair loss.
Hormone therapy, targeted cancer drugs and immunotherapy are more likely to cause hair thinning but can also cause hair loss. Radiotherapy can cause hair to fall out in the area being treated. Hair on other parts of the body is not usually affected.
You may have:
mild thinning of your hair
partial or patchy hair loss
complete hair loss (alopecia)
Complete hair loss can happen gradually. Or hair may fall out fairly quickly, in clumps.
Hair loss or thinning can also affect your eyelashes, eyebrows and other body hair. For example, pubic hair, underarm hair and chest hair in men.
Chemotherapy works by killing dividing cells such as cancer cells. But normal body tissues such as the hair follicles, also have lots of diving cells. This is what makes your hair fall out.
Not all chemotherapy drugs cause hair loss. Some don't cause any hair loss at all or only cause slight thinning. If your hair is going to fall out, it usually begins within 2 to 3 weeks after treatment starts.
Hair usually grows back once your treatment has finished. However, in some people, it may not grow back or it might grow back patchy. This usually only happens with very high doses of particular drugs.
It might take several months for the hair to grow back. When it does, it might look the same as before, or it may be thicker or thinner. Sometimes it can be a different colour or curlier.
There are different types of targeted cancer drugs and immunotherapy that can cause hair problems. Some of these drugs cause slower hair growth, hair thinning and dry, brittle hair. Some might cause complete hair loss.
A type of targeted cancer drug called epidermal growth factor receptor (EGFR) inhibitors can cause permanent hair loss. But this is usually when you have it long term.
Instead of hair loss, some targeted cancer drugs cause hair growth in unexpected areas of the body. For example, excessive hair on the face or very long, curly eyelashes.
Talk to your doctor or nurse if your treatment is causing excessive hair growth. Ask about the safest way to remove unwanted hair. For example, you (or someone else) might need to carefully trim your eyelashes every few weeks to stop them from irritating your eyes.
Hormone therapies are more likely to cause hair thinning than hair loss. An example of this is a drug called tamoxifen for breast cancer.
Ask your doctor or specialist nurse if the drugs you are having are likely to cause hair thinning.
Check the name of the cancer drug treatment with your doctor or nurse, then find out about it on our A to Z list of cancer drugs.
Radiotherapy to the brain always causes some hair loss. If you are having treatment to a particular part of the head, your hair only falls out in that area. You might also have some hair loss on the opposite side of the head, where the radiotherapy beams pass through. This area is called the exit site.
Whether or not your hair grows back depends on the type of radiotherapy you're having. For example, if you're having whole brain radiotherapy to treat your symptoms it's likely that your hair will grow back. Whereas treatment to try to cure cancer uses a high dose of radiation and so permanent hair loss is much more common.
It might take more than 6 months after radiotherapy for your hair to grow back. If your hair does grow back it may not be quite as thick as before and in some people can be patchy.
Read more about radiotherapy treatment
Your doctor suggests the best treatment for you. But sometimes there is a choice of drugs you can have.
Speak to your doctor if you find the thought of losing your hair very upsetting. They might be able to suggest a treatment less likely to cause hair loss.
Your doctor might also talk to you about ways of reducing hair loss from chemotherapy treatment. They may suggest you try scalp cooling.
Unfortunately, there is no known way to prevent hair loss from:
radiotherapy
hormone therapy
targeted cancer drugs
immunotherapy
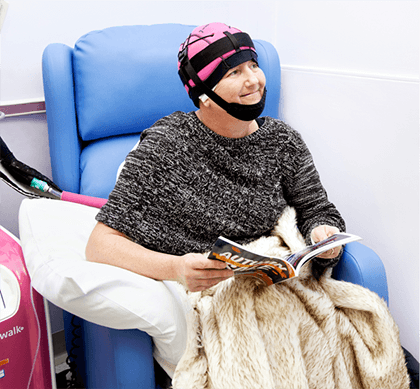
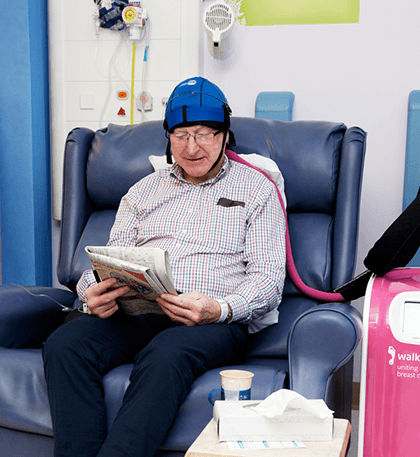
Scalp cooling can sometimes reduce the amount of hair loss.
Scalp cooling lowers the temperature of your scalp and reduces the blood flow in the scalp. This reduces the amount of chemotherapy that reaches the hair follicles on your head. With less of the chemotherapy drugs getting to the hair follicles, the hair is less likely to die off and fall out.
There are different types of scalp cooling. These include:
cold cap. This is a hat filled with a gel that is chilled before you put it on
refrigerated cooling system. You wear a cap that is attached to a machine that pumps liquid coolant into the cap
You can ask your doctor or nurse if your hospital has scalp cooling and which type they use. They can explain exactly what happens.
Scalp cooling is not suitable for everyone. You won’t normally have scalp cooling if there is a high risk that there might be cancer cells in your scalp. Scalp cooling is also not recommended for people:
with blood cancers such as leukaemia and lymphoma
who are going to have scalp radiotherapy
You would not have scalp cooling with continuous chemotherapy through a pump or with chemotherapy tablets. This is because you would have to wear the cold cap for 24 hours a day.
Scalp cooling only blocks certain chemotherapy drugs and doesn't work for everyone. So you might still have hair thinning, or lose your hair completely. We can only tell whether it will work for you once you try it.
Your doctor might not suggest scalp cooling if they are worried about the risk of cancer cells being left on the scalp. This can lead to cancer spread in the scalp (scalp metastases).
Researchers did a of studies in 2018. The review showed that the risk of cancer spreading to the scalp after using a cold cap was very small.
You stay at the hospital for longer if you have scalp cooling. You need to wear the cap before, during and after you have the chemotherapy drugs into your bloodstream.
The time varies depending on the drug and type of cold cap system your hospital has. For the Paxman scalp cooling system, you might wear the cap:
for about 30 to 45 minutes before treatment depending on your hair type
during treatment for as long as it takes to receive the drugs
after treatment for a minimum of 20 to 90 minutes depending on the drugs you have had
Your nurse might ask you to dampen or wet your hair before you put on the cap or cooling system. This is to improve contact between the scalp and cap and lower the temperature of the skin on your scalp. You also have a small amount of conditioner added to help in removing the cap after you have finished treatment.
Research suggests that scalp cooling with Afro Caribbean hair is not as successful. So your nurse might recommend you have longer periods of scalp cooling if this applies to you.
Scalp cooling can make you feel cold all over and uncomfortable. At the start, you might feel very uncomfortable for around the first 15 minutes. This should then ease. Let your nurse know if you can’t cope and want to stop the treatment. Scalp cooling can also:
give headaches or pain in your forehead
make you feel sick
make you feel dizzy and lightheaded
take extra layers to put on
take or ask for a blanket
drink hot drinks to help you feel warmer
ask for some painkillers before the scalp cooling starts
Read about coping with hair loss
This page is due for review. We will update this as soon as possible.
Last reviewed: 02 Mar 2023
Next review due: 02 Mar 2026
Hair loss due to cancer treatment can be very stressful. There are some practical things you can do to help.
Read about the different types of wigs, whether you can get one through your health service, and tips on how to wear them.
Find out about different ways to cover your head, including hats, scarves, turbans and stretchy tubes.
Learn skin care and make up tips to help you feel better.
Coping with cancer can be difficult. There is help and support available. Find out about the emotional, physical and practical effects of cancer and how to manage them.
Cancer and its treatment can change how you look. This might affect how you feel about yourself.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.