Smoking, tobacco and cancer
Smoking causes at least 16 different types of cancer and is the biggest cause of lung cancer in the UK, and worldwide. Smoking causes other diseases too, such as heart disease and various lung diseases.
If you smoke, stopping completely is the best thing you can do for your health.
Both the amount you smoke, and the length of time you’ve been smoking for, affect your cancer risk.
The more cigarettes you smoke a day, the higher your risk of cancer. So reducing the number of cigarettes you smoke a day is a good first step.
But the number of years you smoke for affects your cancer risk the most. So it’s important to make a plan to stop smoking completely.
The sooner you stop, the lower your risk of cancer. Everyone who smokes can benefit from stopping, and it’s never too late to stop - even if you’ve smoked for years. Speak to your doctor or pharmacist, free local stop smoking service, or visit NHS Smokefree to get support on how to stop smoking for good.
Find out more about how to stop smokingThe link between smoking and cancer is very clear. It causes at least 16 different types of cancer, including two of the most common types: lung cancer and bowel cancer.
Cancers caused by smoking include:
nose and sinuses
mouth
pharynx (upper throat)
larynx (voice box)
oesophagus (food pipe)
lung
breast
liver
stomach
kidney
pancreas
bowel
ovary
bladder
cervix
some types of leukaemia
Smoking causes cancer in multiple ways. The main way is by damaging the DNA in our cells.
DNA controls how our cells grow and behave. Damage to DNA causes cells to behave in ways that they’re not supposed to. And the build-up of DNA damage over time can lead to cancer.
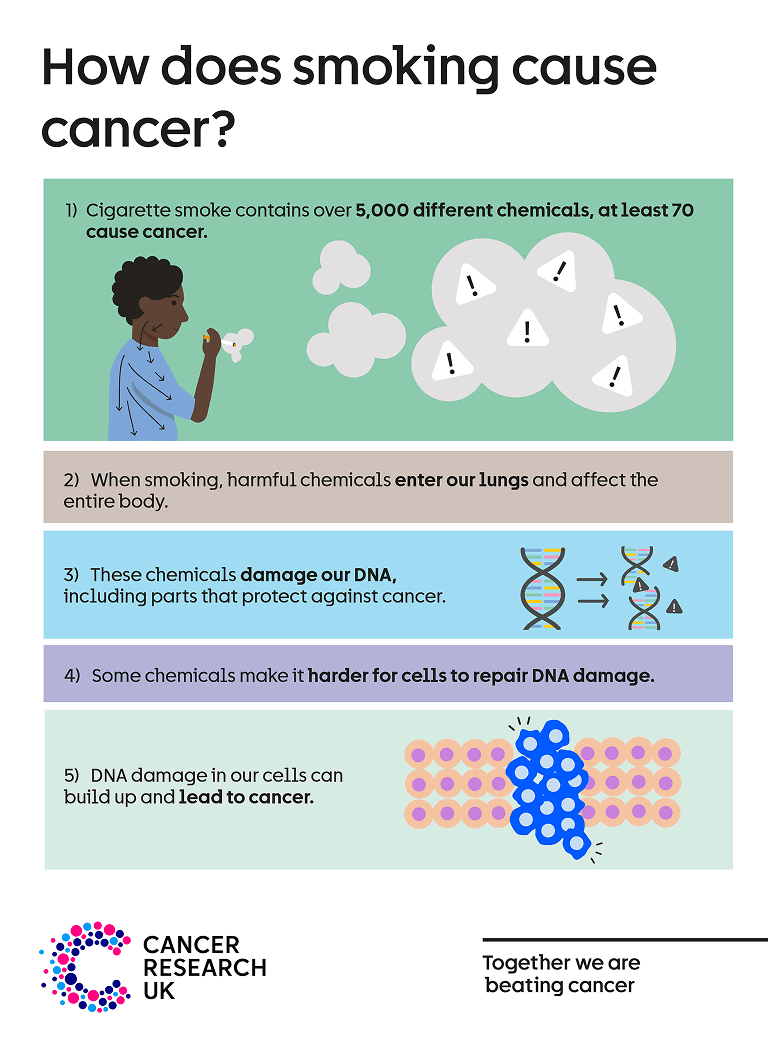
Cigarette smoke contains over 5000 chemicals and many of these are harmful - we know at least 70 can cause cancer.
When smoking, the harmful chemicals enter our lungs and affect the entire body.
These chemicals damage our DNA, including parts of our DNA that protect us against cancer.
Chemicals in cigarette smoke also make it harder for our cells to repair DNA damage. This means DNA damage can build up.
It’s the build-up of DNA damage in the same cell over time that leads to cancer.
You can find more information on the chemicals in cigarettes that cause cancer and what smoking does to the body on our webpage.
Smoking is the biggest cause of lung cancer. And lung cancer is the most common cause of cancer death.
Smoking causes more than 6 in 10 lung cancer cases in the UK. Both active smoking and passive smoking cause lung cancer. Passive smoking is when a person breathes in someone else’s tobacco smoke. You can find out more about passive smoking on our webpage.
There are some other things that increase your risk of lung cancer, which you can learn more about on our causes of lung cancer page.
People who smoke sometimes have a cough. But coughing can be a sign of lung cancer, as well as other health conditions. If you have a persistent cough, breathlessness or any other symptom that’s new for you or won’t go away, it’s important that you tell your doctor about it. If you have any doubts, don’t ignore it.
Remember, it’s never too late to stop smoking and reduce your risk of lung cancer. The best way to reduce your risk is to stop smoking completely.
Our tips and support to help you stop smoking for good.
Yes, ‘light’, ‘occasional’, or ‘social smoking’ still increases your risk of cancer.
Even smoking fewer cigarettes than 1 a day increases the risk of dying early, compared to people who have never smoked. And studies looking at people who smoke fewer than 10 cigarettes per day show an increased risk of smoking-related cancers and other diseases.
Reducing the number of cigarettes you smoke a day is a good first step. But, there is no safe level of smoking. The best thing you can do for your health is to stop smoking completely, and it is never too late to stop.
Find out more about how to stop smokingLast reviewed: 07 Jun 2023
Next review due: 07 Jun 2026
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.