Radiotherapy
Internal radiotherapy gives a high dose of radiation to the cancer but very little to the surrounding tissues.
You usually have internal radiotherapy to give an extra dose of radiation after external radiotherapy. In some situations, you might have internal radiotherapy on its own, but this is not very common.
You might have treatment in the radiotherapy department as an outpatient. Or you might stay in hospital. This depends on the type of treatment you have.
There are 2 types of internal radiotherapy for vaginal cancer. These are:
intracavity radiotherapy – you have treatment through a plastic tube (applicator) in the vagina
interstitial radiotherapy – you have treatment through thin tubes which a surgeon places into the cancer
Your doctor will explain what will happen during your treatment. The radiographers and nurses are also an important part of your treatment team. Do speak to them if you have any questions or concerns.
You usually have between 2 to 4 treatments. Your or doctor will tell you how many treatments you need and when you have them.
The radiotherapy team plans your internal radiotherapy before you start treatment. This means working out exactly where in your vagina you need treatment. You might have planning and your first treatment at the same appointment. Or you might have planning and then come back for your treatment on another day.
Your radiographer will ask you to empty your bladder, and then takes you into the treatment room. You undress from the waist down and put a gown on. You then lie on a couch.
Your doctor examines your vagina. This is to check what size applicator you need for your treatment. The applicator is a plastic tube similar to a tampon. It comes in different sizes.
The doctor inserts the applicator into your vagina. A clamp holds it in place. The doctor or radiographer uses to help insert the applicator. This makes it as comfortable as possible.
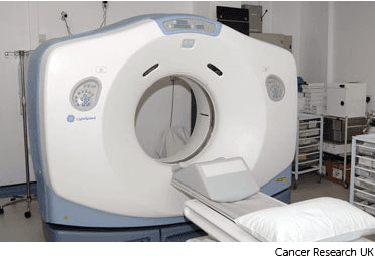
You then have a which takes a few minutes. The radiographers wait outside while this happens. Your doctor uses the results of the CT scan your plan your treatment.
Sometimes you may also have an to help plan your treatment.
The applicator remains in place if you have treatment on the same day. This starts soon after the CT scan. They remove the applicator if you are having your treatment on a different day. Your radiographer will let you know when you need to come back.
You are in the same position as you were for the CT scan. The doctor or radiographer inserts the applicator into your vagina. They then connect it to the brachytherapy treatment machine.

The radiographers leave the room during treatment, but they can see you via a CCTV screen. They operate the treatment machine from outside the room.
A small radioactive pellet called a source passes from the machine into the applicator. The source gives a dose of radiotherapy into the vagina. At the end of the treatment it returns to the treatment machine.
Each treatment takes up to 20 minutes.
The treatment isn’t usually painful, but the applicator might be uncomfortable. You can have pain relief if you need it.
The radiographers remove the applicator once treatment is complete. You are then free to go home.
You are only radioactive when the treatment machine is switched on. So after each treatment, you are safe to be around everyone, including children.
You stay in hospital for a few days to have this. You may have treatment twice daily over a few days or once weekly.
You usually go into hospital on the morning of your treatment or the day before. You go to the operating theatre and have an . The anaesthetic might be:
an injection into your spine (epidural) so you feel nothing below the waist
a general anaesthetic that puts you to sleep
The doctor places narrow tubes called applicators into the cancer within the vaginal wall. They may place gauze inside your vagina so the applicators don’t move. They may use a vaginal applicator at the same time. Exactly how you have the treatment depends on your planning scan.

When you wake up you usually have a CT scan or MRI scan or you might have both. This is to check the position of the applicators and to plan your treatment.
Once the applicators are in place, you cannot leave the bed and must remain flat. The doctor will put a tube into your bladder (urinary catheter) to collect your urine. You will have tablets to stop you needing to poo. If you do need to poo, your nurse will help you to use a bed pan.
The radiographer will explain how often and how long your treatments will be. This depends on your treatment plan.
For each treatment you go to the brachytherapy treatment room in the radiotherapy department. The radiographers connect the applicators to the brachytherapy treatment machine.
They leave the room during treatment, but they can see you via a CCTV screen. They operate the treatment machine from outside the room.
A small radioactive pellet called a source passes from the machine into the applicator. The source gives a dose of radiotherapy into the vagina. At the end of the treatment it returns to the treatment machine.
You can have visitors when you are not having treatment.
Tell your nurse or doctor if you are in pain or have any discomfort. They can give you regular pain relief.
After your treatment you may have a and your doctor removes the applicators. You might need some pain relief for this. They also take out your urinary catheter.
You might be able to go home that day or stay overnight, depending on how you feel. You will need someone to stay with you at home for 24 hours.
The most common side effects usually happen shortly after having treatment. They may last for a couple of weeks. There is a risk of late side effects that happen months or years after having treatment.
Your treatment team goes through all the side effects before you start treatment. Tell them if you develop any side effects so that they can help you manage them.
You might have some vaginal bleeding or straight after treatment. Your vagina might also be sore or inflamed. Use sanitary towels rather than tampons for any bleeding or discharge. This is to reduce the risk of infection.
Contact your advice line if the discharge smells unpleasant or if the bleeding is heavy.
You may notice that your poo becomes softer or you might have . Let your doctor know if you have this. They might give you medicines to help control it. Drink plenty of fluids to replace the liquid you have lost.
The treatment can inflame the lining of the bladder. This is called radiation cystitis.
It can make you very uncomfortable. You might have a lot of bladder pain or a burning feeling when you pee. It may feel as though you need to pee all the time, even though you know you’ve only just been. Try to drink plenty of fluids because this can help.
Speak to your healthcare team if you have pain or feel you need to pee more often.
You might feel tired during your treatment and for a few weeks after. You might also feel weak and lack energy. Rest when you need to.
Various things can help you to reduce tiredness and cope with it, such as exercise. Some research has shown that taking gentle exercise can give you more energy. It's important to balance exercise with resting.
Find out more about tiredness and fatigue and how to cope with it
In the long term, internal radiotherapy can reduce the amount of natural fluid in the vagina. This might make it feel dry and uncomfortable. There are gels and lubricants available to help improve the dryness.
Ask your radiographer or nurse what you can use.
In the long term, your vagina may become shorter, narrower, and less stretchy. This is called fibrosis. Having sex and vaginal examinations in the future can become uncomfortable.
To try to prevent this, your radiographer or nurse will give you vaginal dilators to use after your treatment. They will explain how you should use them.
Speak to your doctor or nurse if you have any problems or questions, or if you don’t feel comfortable with using dilators for any reason.

The radiotherapy staff may be able to arrange transport if you have no other way to get to the hospital. Your radiotherapy doctor would have to agree. This is because it is only for people that would struggle using public transport and have no access to a car.
Some people are able to claim back a refund for healthcare travel costs. This is based on the type of appointment and whether you claim certain benefits. Ask the radiotherapy staff for more information about this.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Last reviewed: 28 Aug 2025
Next review due: 28 Aug 2028
Vaginal cancer is when abnormal cells in the vagina start to divide and grow in an uncontrolled way.
Radiotherapy uses high energy waves similar to x-rays to kill cancer cells.
Your treatment depends on a number of factors including the type and stage of cancer and where the cancer is in your vagina.
There is support available to help you cope with a diagnosis of cancer, life during treatment and life after cancer.
Vaginal cancer is very rare. It starts in the vagina, which is the passage that leads from the neck of the womb (cervix) to the vulva. Vaginal cancer is more common in older women.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.