Tests and scans
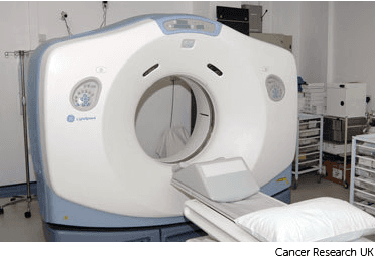
A CT colonography is a test to look at your large bowel (colon) and your back passage (rectum). The test uses CT scans to show the inside of your colon and rectum.

You have this test as an outpatient in the CT scanning or radiology department at the hospital. A or specialist doctor called a radiologist does the test.
The test takes around 20 minutes, but you are usually in the department for about an hour.
You usually have this test to help find the cause of your symptoms.
You need to have an empty bowel for this test. This is so the radiographer can clearly see the inside of your bowel and rectum.
You'll get written information on what to do before you have a scan. Your preparation usually starts a couple of days before the test.
You usually take to help empty your bowel the day before. Or you might need to drink a special liquid called gastrografin over 1 or 2 days.
Gastrografin is a type of dye containing iodine. It helps to make the scan pictures clearer. It also acts as a laxative and may give you diarrhoea.
Having gastrografin or laxatives will mean that you need to open your bowels often, and sometimes very suddenly. You might also have some cramping pains. It’s best to stay at home for a few hours after taking gastrografin or the laxatives, so that you are near a toilet.
You might also need to follow a low fibre diet for 1 or 2 days before the test.
To prevent dehydration, it’s important to drink plenty of clear fluids. You will receive a letter and information from
your healthcare team about what you should eat and drink.
You may need to stop taking iron tablets or other medicines that can cause . You usually stop these about one week before the test. They will also tell you if you need to stop any of your regular medication and how long for.
Contact the radiology department as soon as possible before your appointment if you take medicines to thin your blood or if you are diabetic. You'll get other instructions to follow.
When you arrive, you usually fill out a checklist or questionnaire with the radiographer. They will explain the procedure and ask you to sign a consent form. They ask you questions about your medical history and any allergies. It's a good time to ask them any questions that you may have.
They'll ask you to change into a hospital gown.
You might have a medicine to relax your bowel muscles. This helps to reduce tummy cramps during your test. You usually have it as an injection through a fine tube called a into your bloodstream.
You lie on your side on the CT scan couch.
The radiographer puts a small tube, which is a few centimetres long into your rectum. They then pass carbon dioxide gas or air inside. This opens the bowel and helps to get clear scans of the inside of your bowel. You may feel uncomfortable and bloated. And may feel you need to go to the toilet or pass wind. This is normal but try to keep in as much gas as you can.
You might have more carbon dioxide gas passed into your bowel during the test to keep the bowel open.
This 2 minute video shows how you have a CT colonography.
When you have the right amount of gas in your bowel, you have the CT scan. This is usually taken with you lying in 2 or 3 different positions. This is to make sure the whole bowel is seen clearly. You will be alone in the room while you have the scan. But your radiographer can still see you and talk to you through an intercom.
During the scan, you might have an injection of contrast medium. This helps show up the bowel more clearly on the scans. You have this through your cannula.
At certain times, the radiographer may ask you to hold your breath for a few seconds. It is important that you lie as still as you can during the scan.
A computer matches all the scans you've had to make a virtual scan of the inside of your bowel.
After the scan the radiographer removes the tube from your back passage and shows you to the toilet. You usually stay in the department for about 20 to 30 minutes after the test. This is to check you don't have an allergic reaction to the medication you’ve had.
The radiographer will remove the cannula from your vein when it’s time for you to go home. You can usually eat, drink, and take your medicines as normal after the scan.
CT colonography is a safe procedure. Your radiographer will tell you who to contact if you have any problems after your test. Your doctor will make sure the benefits of having a CT colonography outweigh the possible risks.
Some of the possible risks include:
Clearing the bowel can cause dehydration in some people. It is very important to drink plenty of fluids before and after your scan.
Gastrografin can make people feel or be sick. It may cause a mild rash but this is uncommon. Very rarely you can have an allergic reaction. If you feel ill or have problems breathing during the test, tell the radiographer straight away.
The injection of contrast medium might make you hot and flushed for a few minutes. And you might get a metallic taste in your mouth. You might also feel like you’re passing urine, but you aren’t – this feeling can be quite common and should pass quite quickly.
Very rarely, people can have a reaction to the contrast medium. Tell the radiographer straight away if you feel ill or have problems breathing during the test.
You may have some bloating or pain in your abdomen after the test. This is due to the carbon dioxide or air put into the bowel. This should go away shortly afterwards.
There is a small risk of a tear (perforation) in your bowel. This is very rare. If it happened, you would often need surgery to repair the tear.
You might have temporary blurred vision if you had medicine to relax your bowel. You shouldn't drive for at least an hour or so or until your vision has returned to normal.
Tell your radiographer if you have glaucoma or heart problems before you have medicine to relax your bowels.
Rarely might you feel faint after having the muscle relaxant.
CT scanners use x-rays to make images which use a small amount of radiation. Exposure to radiation during a CT scan can slightly increase your risk of developing cancer in the future. Talk to your doctor if this worries you.
You should not have CT colonography if there is a risk that you are pregnant.
Read our information on ionising radiation and cancer risk
It can take up to 1 to 2 weeks to get your results. You usually get your results from your specialist. It is important to check with your doctor how long you should expect to wait for your results.
Waiting for test results can be a worrying time. You might have contact details for a specialist nurse. You can get in touch with them for information and support if you need to. It may help to talk to a close friend or relative about how you feel.
If you have not had your results a few weeks after your test, you could contact your doctor to chase your results for you.
We have more information on tests, treatment and support if you have been diagnosed with cancer.
Last reviewed: 14 Apr 2025
Next review due: 04 Apr 2028
You might have a number of tests to check for bowel cancer. This includes a test that looks for tiny traces of blood in a sample of poo (FIT) and a test to look at the inside of your bowel (colonoscopy).
Find out about tests to diagnose cancer and monitor it during and after treatment, including what each test can show, how you have it and how to prepare.
A CT scan is a test that uses x-rays and a computer to create detailed pictures of the inside of your body. Find out how you have it and what happens afterwards.
Search for the cancer type you want to find out about. Each section has detailed information about symptoms, diagnosis, treatment, research and coping with cancer.
About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.