Tests and scans
MRI stands for magnetic resonance imaging. An MRI is a type of scan that creates pictures using magnetism and radio waves.
MRI scans produce pictures from angles all around the body and shows up soft tissues very clearly. A operates the scanner and looks after you while you have your scan.
It is a safe test. If you have an injection of contrast dye it can cause a headache, dizziness or a warm flushed feeling.
An MRI scan can be used to look at most areas of the body and is used to:
find a tumour
find out how big it is and whether it has spread (stage a cancer)
measure blood flow
to check how well treatment is working
You might have an injection of a special dye called a before the scan. This is to help make the scan pictures clearer.
MRI scans are particularly good for:
brain tumours
primary bone tumours
soft tissue sarcomas
tumours affecting the spinal cord
tumours in the pelvic organs, including prostate, bladder, womb and ovarian tumours
Read about different cancer types in our A - Z list
In some situations, your doctor may suggest an MRI scan if a CT scan hasn't been able to give all the information they need.
In some cancers, an MRI can be better than CT scans at showing how deeply the tumour has grown into body tissues. It can be particularly useful for showing whether the tissue left behind after treatment is cancer or not.
Your appointment letter will list any special instructions. For most MRI scans, there is no special preparation beforehand. But for some, you might have to stop eating a few hours before your test. This depends on which part of the body you are having scanned.
Take your medicines as normal unless your doctor tells you otherwise.
You might need a blood test to check your kidney function. Your MRI team will let you know if you need this.
Before you go to your appointment, or when you arrive, you fill in a safety checklist. This asks about:
any operations you’ve had
whether you have any metal implants or other metal in your body
any allergies you may have
An MRI scan uses strong magnetism which could affect any metal in your body. This includes:
pacemakers or an implantable defibrillator (to treat abnormal heart rhythms)
surgical clips, pins or plates
cochlear implants (for deafness)
metal fragments anywhere in your body – for example, from an injury, dental fillings and bridges
You may still have an MRI scan if you have some metal in your body. But your doctor and radiographer will decide if it’s safe for you. It’s important to tell the scanner staff about any metal in your body.
Some people feel claustrophobic or closed in when they’re having an MRI scan. Contact the department before your test if you’re likely to feel like this. The hospital staff can take extra care to make sure you’re comfortable and that you understand what’s going on. Your doctor can give you medicine to help you relax if you need to.
An MRI is generally safe during pregnancy. But it is important to tell your doctor or the MRI staff beforehand if you think you’re pregnant. They will discuss the risks and benefits with you.
When you arrive at the department the radiographer explains what will happen and asks you to sign a consent form. This is a good time to ask any questions you may have.
Your radiographer might ask you to change into a hospital gown. You might not have to undress if your clothing doesn’t have any metal, such as zips or clips.
You have to:
remove any jewellery, including body piercings and your watch
remove your hair clips
empty your pockets of coins and keys
You might be able to take a relative or friend into the scanning room with you. But check with the department staff first. Your friend or relative will also need to remove any metal they have on them.
Your radiographer takes you into the scanning room. The MRI machine is large and shaped like a doughnut.
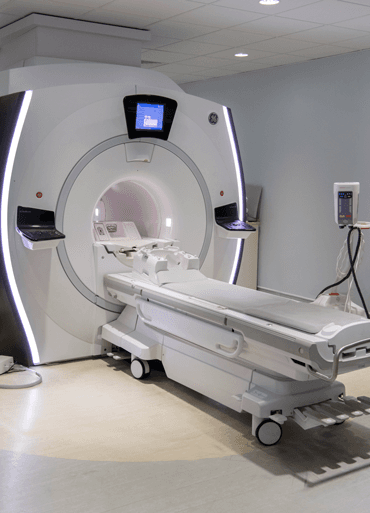
You lie on your back on a couch that can slide into the MRI machine.
You might have an injection of a dye (contrast medium) through a small plastic tube called a cannula into a vein in your arm. This helps to show up your body’s organs more clearly. Some people are allergic to the dye, so your radiographer will check first about any medical conditions or allergies you have.
After the dye injection you may:
feel sick
have a headache
feel warm or flushed
have a metallic taste in your mouth
feel a little dizzy
have a skin rash
These effects are usually mild and last for a short time. Tell your radiographer if you feel unwell at any point during or after your scan.
Once you’re in the right position on the couch, your radiographer leaves the room. They can see you on a TV screen or through a window at all times from the control room. You can talk to each other during the scan, usually through an intercom. You will have a button you can press if you want them to stop the scan immediately if you feel claustrophobic.
You need to lie as still as possible. The scan is painless but it can be uncomfortable to stay still. Tell the radiographer if you're getting stiff and need to move.
The couch moves through the MRI scanner. It takes pictures as you move through it. Your radiographer might ask you to hold your breath at times.
The scanner makes a very loud clanging sound throughout the scan. You wear headphones or earplugs to protect your hearing. You may also be able to listen to music during your scan.
The scan can take between 15 and 90 minutes. It depends on the area that they need to scan and how many images they need.
This 1 minute video shows you what happens when you have an MRI scan.
When the scan is over, your radiographer comes back into the room and lowers the couch so that you can get up.
You usually stay in the department for about 15 minutes after your scan if you've had the dye. This is in case it makes you feel unwell.
Your radiographer removes the cannula from the vein in your arm before you leave.
You should then be able to go home or back to work, and also eat and drink normally.
If you’ve had medicine to help you relax (sedation), you need someone to take you home and stay overnight. If you've had sedation, for the next 24 hours, you also shouldn’t:
drive
drink alcohol
operate heavy machinery
sign any legally binding documents
An MRI is very safe and doesn’t use radiation. Some people can’t have an MRI but the checklist picks this up beforehand. Your doctor and radiographer make sure the benefits of having the test outweigh any possible risks.
Some of the possible risks include:
You might get a small bruise around the area where they put the needle in for the cannula.
There's a risk that the contrast medium will leak outside the vein. This can cause swelling and pain in your arm but it’s rare. Tell your radiographer if you have any swelling or pain. Let your GP know if it doesn’t get better or starts to get worse when you’re at home.
An allergic reaction to the contrast medium injection is rare. This most often starts with feeling weak, sweating and difficulty breathing. Tell your radiographer straight away if you feel unwell so they can give you medicine to control the reaction.
You should get your results within 1 or 2 weeks.
Ask your doctor, radiographer, or nurse how long it will take to get them. Contact the doctor who arranged the test if you haven’t heard anything after a couple of weeks.
Waiting for test results can make you anxious. You might have the contact details of a specialist nurse who you can speak to for information and support if you need to. It may also help to talk to a close friend or relative about how you feel.
We have more information on tests, treatment and support if you have been diagnosed with cancer.
Last reviewed: 28 Apr 2025
Next review due: 28 Apr 2028
Find out about tests to diagnose cancer and monitor it during and after treatment, including what each test can show, how you have it and how to prepare.
A CT scan is a test that uses x-rays and a computer to create detailed pictures of the inside of your body. Find out how you have it and what happens afterwards.
Search for the cancer type you want to find out about. Each section has detailed information about symptoms, diagnosis, treatment, research and coping with cancer.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.