Radiotherapy for oesophageal cancer
Internal radiotherapy gives a high dose of radiation to the cancer but very little to surrounding tissues. This treatment can shrink the cancer and relieve symptoms such as difficulty swallowing. You might have internal radiotherapy on its own or after .
You might have the treatment as a day case. Or you might need to stay in hospital.
The radiotherapy team carefully plans your treatment. They work out exactly where the cancer is in the food pipe and how much radiation you need to treat it. Your planning appointment takes from 1 to 2 hours.
Your radiographer gently puts a soft, flexible tube called a nasogastric tube up your nose. It goes down into your food pipe. They might spray your throat beforehand to numb it.
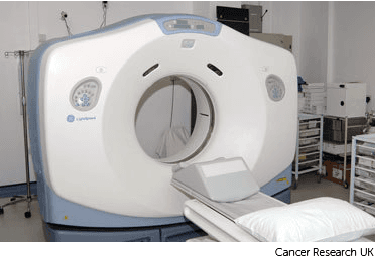
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
The radiotherapy staff take you to the brachytherapy treatment room. They connect the nasogastric tube to the treatment machine.
The staff leave the room. They operate the treatment machine from outside the room.
A small radioactive pellet called a source passes from the machine into the nasogastric tube. The source stops in the area of the cancer to give a dose of radiotherapy. At the end of the treatment it returns to the treatment machine.

The treatment usually takes up to 30 minutes. It doesn’t hurt but the tube can be uncomfortable. You need to lie still.
The staff can see you on a CCTV screen. They are in the next room and can hear you. So you can tell them if you need anything.
The staff come back into the room and gently remove the nasogastric tube. You can usually go home shortly after the treatment.
If you had an anaesthetic spray to numb your throat you mustn’t eat or drink anything for 4 hours. The staff will give you further instructions as necessary.
You might have just one treatment or another treatment after a week or so.
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children.
You might have some soreness when you swallow for up to 2 weeks. Eating softer foods can help. Your nurse or doctor will give you painkillers to reduce the soreness. Let them know if the pain gets worse or lasts for longer than 2 weeks.
You may feel sick (nauseous), although this is usually mild. You might have some anti sickness medicines to take home.
Your food pipe might become narrower and less stretchy over some months or years. This is called an oesophageal stricture. It can make it difficult for you to swallow.
Your doctor can stretch the food pipe slightly. They call this oesophageal dilatation. You have a medicine to make you sleepy (sedation).
Your doctor puts a tube called an endoscope down your throat. It has an area on it called a balloon. Your doctor expands the balloon to widen the food pipe. They repeat this a few times until the narrowing has gone.
It stretches the food pipe so you can swallow more easily again. You might need to have this repeated if the narrowing happens again.

Last reviewed: 21 Sept 2023
Next review due: 21 Sept 2026
Radiotherapy uses high energy waves similar to x-rays to destroy oesophageal cancer cells.
You might have surgery, radiotherapy or chemotherapy or a combination of these treatments. This depends on a number of factors including the stage and type of your oesophageal cancer.
Coping with cancer can be difficult. Help and support are available. There are things you can do and people who can help you cope with a diagnosis of oesophageal cancer.
Oesophageal cancer can cause problems with swallowing and make it hard to eat well. It’s important to eat and drink enough calories and protein to maintain your weight and strength.
Advanced oesophageal cancer means that a cancer that began in the food pipe (oesophagus) has spread to another part of the body.
Oesophageal cancer starts in the food pipe, also known as your oesophagus or gullet. The oesophagus is the tube that carries food from your mouth to your stomach.

About Cancer generously supported by Dangoor Education since 2010. Learn more about Dangoor Education
Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Connect with other people affected by cancer and share your experiences.
Questions about cancer? Call freephone 0808 800 40 40 from 9 to 5 - Monday to Friday. Alternatively, you can email us.