Living with a stoma after treatment for vaginal cancer
You might need to have an operation to create a stoma if your cancer has spread to your bowel or bladder and you need part, or all of these organs removed.
A stoma is an opening in the tummy created during surgery. There are different types of stoma. You might have:
-
a colostomy - an opening of the large bowel onto the tummy
-
an ileostomy - an opening of the small bowel onto the tummy
-
a urostomy - an opening of the urinary system onto the tummy
When you have a stoma, you need to wear a bag to collect your poo or pee.
Some people have a temporary colostomy or ileostomy made during their treatment for vaginal cancer. It is closed a few months later when the bowel has fully healed. Some people have a permanent colostomy or ileostomy.

Getting used to a stoma
It can take a while to get used to dealing with a stoma. Your stoma nurse can give advice and support. So you'll have help both practically and emotionally. As you learn to manage your stoma, it should have less impact on your day to day life.
Eating when you have a colostomy or ileostomy
It normally takes about 6 to 8 weeks for the bowel to settle down after surgery. After this, most people can start eating the foods they used to have before their operation. Your stoma nurse will give you advice about what you can eat and drink shortly after your operation and in the long term.
When going back to your normal diet, it's a good idea to introduce one food a day at first. You can keep a food diary and make a note if a particular food causes cramps or diarrhoea. If so, you can try it again in a few weeks to see if it has the same effect.
Eating with a colostomy
Generally you can eat what you like. Some people may find that particular foods cause problems such as wind, a bad smell or looser poo. Foods that one person finds troublesome may not have the same effect on another. So it's often down to trial and error to find out if a particular food disagrees with you. You can try the food again in a few weeks to see if it's still causing a problem. Once your bowel settles down, you can gradually increase the amount of fibre in your diet. This will help your stool to be more formed.
Eating with an ileostomy
The small bowel is narrower than the large bowel. So some foods such as celery, tough fruit skins, nuts and mushrooms, may cause a blockage. This is usually only temporary but can cause pain and cramps. When you start to eat these types of foods again, try eating them in small portions and chew them really well. You lose more fluid through an ileostomy, so it's important to drink plenty.
Stoma bag smells
If the stoma bag smells it could be due to the bag not fitting properly or it could be due to diet. There are anti odour products that can help.
Having the right colostomy bag to help stop smells
Stomas are different shapes and sizes. So, some bags may not fit you and others will. If the bag doesn't fit properly you are likely to have problems with smell and possible leakage. You could get in touch with a stoma nurse at your hospital. They can get different types of bags for you to try. And they will help you fit them. If you don't have a stoma nurse, ask your GP or surgeon to refer you. You might have to try a few bags before you find the one that suits you best.
Some bags have charcoal filters built into them. Charcoal is good for absorbing smells. The filter lets gas escape from the bag so that it doesn't get too full and uncomfortable. If the bag fits properly you should only be aware of the smell when you are changing or emptying the bag.
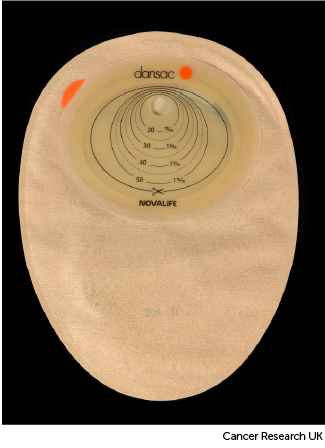
This picture shows what a colostomy bag can look like. There are others available so it may not look exactly like this one.
Anti odour products
Some products can help to mask the smell from a colostomy or ileostomy. They are often liquids, and you use a few drops each time you change your bag. You may not need to use these, but some people have difficulty finding the perfect fit for their colostomy bag and these products can help. You can ask your stoma nurse or the Colostomy Association to suggest products for you.
Rectal discharge
After having a colostomy or ileostomy, you may have mucus coming out of the back passage (rectum). This is from the lining of the bowel. Mucus normally keeps the bowel moist and helps the poo (faeces or stools) to pass along the bowel. After a colostomy or ileostomy, although the bottom part of the bowel no longer has poo passing through, it still produces mucus.
The mucus may leak out of the  , or you may feel the urge to go to the toilet. The mucus is normally clear or white and looks a bit like egg white or glue. Sometimes the mucus dries up into a ball inside the rectum and can cause pain. Depending on the type of stoma you have, a small amount of poo may pass into the bottom part of the bowel, resulting in a brown discharge.
, or you may feel the urge to go to the toilet. The mucus is normally clear or white and looks a bit like egg white or glue. Sometimes the mucus dries up into a ball inside the rectum and can cause pain. Depending on the type of stoma you have, a small amount of poo may pass into the bottom part of the bowel, resulting in a brown discharge.
How often and how much mucus there is varies in different people. It may be once every few weeks or months, or a couple of times a day. If the mucus looks green, smells or has blood in it, you should let your stoma nurse or doctor know as you might have an infection.
Sitting on the toilet every day and gently bearing down (without straining) may help you to pass the mucus out of your rectum naturally. Some people may need a suppository to help loosen the mucus. If you are worried about leaking discharge, you may want to wear a small absorbent pad to protect your clothes.
If mucus does leak out, it can make your skin sore. So you may want to use a barrier cream to help protect your skin. If you are having radiotherapy, you should check with the team looking after you, before using any creams. After a shower, remember to pat your skin dry with a towel rather than rub it.
Although having this can feel embarrassing, the team looking after you will be very used to supporting people with this. Your stoma nurse can give you advice on what to expect and how to deal with any discharge. They can also teach you pelvic floor exercises to help strengthen the muscles that help to control the leakage from the rectum.
Emptying your urostomy
You will need to empty your urostomy bag every few hours. So you will need access to a toilet.
So you don’t have to keep getting up at night, you can connect your urostomy bag to a larger night bag. This can attach to your leg, or you can have it by your bed.
If you are travelling or on a long car journey, you might also want to take a night bag. You can use this if you can’t access a toilet.
Mood and body image
It is normal to feel worried about how you will look if you need to have a stoma. You may also worry about how other people react. While you are in hospital the stoma nurse will teach you how to manage the stoma. It might be helpful for a close family member to be there too. Then you can both get used to your stoma and can ask the nurse questions.
Once you get home, help is still available if you need it. You might have problems or questions about looking after your stoma. Or you may feel low or depressed. Do talk to your GP or stoma nurse. They will either be able to help you or put you in touch with someone who can.
Your job
Having a stoma should not make any difference to your job unless it involves heavy manual work. You will need to have easy access to a toilet. If you are not sure about this, ask your stoma nurse for advice.
Sports and hobbies
The stoma won't stop you enjoying your favourite pastimes. All sorts of physical activities are possible – even strenuous exercise and swimming. Your stoma nurse can give you advice on how to protect your stoma. They can also tell you about waterproof bags and seals for swimming and water sports.
Relationships and sex life
You might worry about how the stoma will affect your relationships with a partner or with friends. Or have practical worries about the stoma bag being noticeable, leaking or smelling.
Stoma bags are very well designed. They can't be seen through clothes and shouldn't smell or leak.
Many people find that it helps if they talk openly to close family and friends. Most people want to understand what is happening so they can help you.
Radar key and just can't wait card
Many people worry about having access to a toilet when they’re out. There are special keys called radar key’s you can get that gives you access to thousands of toilets in the UK. It also tells you where they are.
Also, you can get a just can't wait card, this gives you peace of mind and access toilets in a rush.
Speak to your specialist nurse about getting a radar key or just can't wait card.



