Chemotherapy for acute lymphoblastic leukaemia (ALL)
Chemotherapy uses anti cancer (cytotoxic) drugs to destroy cancer cells. The drugs circulate throughout the body in the bloodstream.
Chemotherapy is the main treatment for acute lymphoblastic leukaemia (ALL). You have several different chemotherapy drugs over a few days. Many people find having a copy of the treatment timetable very helpful. You may have treatment as part of a clinical trial.
Your exact treatment depends on a number of factors such as your type of ALL, age and level of fitness. But you can usually divide it into phases. The names of the phases of ALL treatment aren't very important. They have been this way for a long time. But it's good to know what your treatment team might be referring to when they explain your treatment to you. These are:
- steroid pre phase
- induction
- consolidation
- intensification
- maintenance
You start chemotherapy in the induction phase of your treatment.
You might have other treatment alongside chemotherapy. We have more information about the treatments you might have in each phase.
Induction
The aim of the induction phase is to destroy as many leukaemia cells as possible. After treatment, your doctor calls it a complete remission (CR) if:
- there is no sign of leukaemia in your
bone marrow  when looked at under a microscope
when looked at under a microscope - your blood count has returned to normal
What treatment do I have?
You start treatment quite quickly after getting diagnosed and you have several chemotherapy drugs over a few days.
Chemotherapy damages healthy bone marrow cells as well as the leukaemia cells. So you will generally need to stay in hospital until you have recovered. This is usually about 4 to 6 weeks.
Some of the chemotherapy drugs you might have include:
- vincristine
- doxorubicin
- cyclophosphamide
- cytarabine
- asparaginase
- methotrexate
We have specific information about each of these drugs on our cancer drugs A to Z list.
Chemotherapy into the fluid around the spinal cord and brain
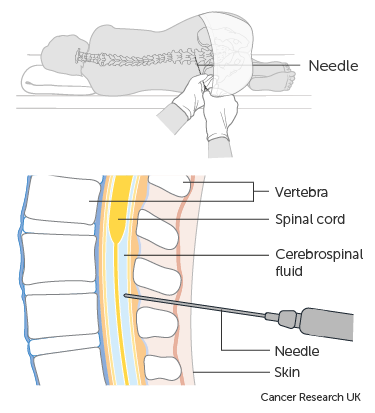
Leukaemia cells can sometimes travel to the brain and spinal cord (the central nervous system or CNS). So as part of your induction treatment your doctor injects chemotherapy directly into the fluid that circulates around the spinal cord and brain. This is called intrathecal chemotherapy.
You have intrathecal chemotherapy to prevent leukaemia cells spreading to the CNS (CNS directed prophylaxis). You have intrathecal chemotherapy during all phases of your treatment.
If you have leukaemia cells in your CNS at diagnosis, you will receive extra intrathecal chemotherapy injections to clear the leukaemia from this area.
You have intrathecal chemotherapy in the same way you have a lumbar puncture.
Steroids alongside chemotherapy
Steroids are naturally made by our bodies in small amounts. They help to control many functions. But steroids can also be made artificially and used as drugs to treat ALL.
You usually have a type of steroid called corticosteroids. These are man-made versions of the hormones produced by the  just above the kidneys.
just above the kidneys.
Corticosteroids include:
- prednisolone
- dexamethasone
- methylprednisolone
- hydrocortisone
You usually start taking steroids for up to a week before you start chemotherapy for induction treatment. Steroids are very good at getting rid of the leukaemia cells. It also gives your doctor time before starting chemotherapy to get the results of important genetic tests. These results help them to plan your treatment.
Targeted cancer drugs alongside chemotherapy
If you have Philadelphia positive ALL you have a type of targeted cancer drug called a  alongside your chemotherapy treatment. Most commonly, this is imatinib (Glivec). You take this as a tablet every day. This will continue throughout all your treatment.
alongside your chemotherapy treatment. Most commonly, this is imatinib (Glivec). You take this as a tablet every day. This will continue throughout all your treatment.
You can watch this short video that explains what Philadelphia positive ALL is.
The human body is made up of trillions of cells. Inside each cell is a nucleus and within the nucleus are the cell’s chromosomes. There are 23 pairs in total.
Chromosomes are made up of DNA, which gives the instructions that tell a cell what to do. Sections of DNA are called genes. They carry the information that makes you you. For example, they tell your body what colour your hair will be or what colour your eyes will be.
Genes also tell your cells when to divide and grow, and when to die.
When cells divide to make new cells, they make exact copies of the chromosomes.
In Philadelphia chromosome positive leukaemia an abnormal change happens to chromosomes 9 and 22. Part of chromosome 9 breaks off where the gene ABL1 is located and part of chromosome 22 breaks off where the BCR gene is located. The broken parts swap places creating a new gene on chromosome 22.
This new chromosome is called the Philadelphia chromosome and the new gene is called BCR-ABL1. This new gene tells the cell to make a large quantity of a protein called tyrosine kinase which encourages leukaemia cells to grow.
There are targeted cancer drugs that can block the protein and stop the leukaemia from growing. These drugs are called tyrosine kinase blockers. You take them as tablets.
For more information about your type of leukaemia and treatments go to CRUK.org/about-cancer/leukaemia.
Consolidation and intensification
The aims of these phases are to get rid of any leukaemia cells that might still be there and to reduce the risk of the leukaemia coming back.
In these phases you're likely to have some of the same chemotherapy drugs you had in the induction phase. You will also have some others. You usually have higher amounts (doses) of the drugs so the treatment is stronger.
Common chemotherapy drugs for these phases include:
- doxorubicin
- asparaginase
- methotrexate
- cytarabine
- etoposide
- daunorubicin
- cyclophosphamide
- mercaptopurine
We have specific information about each of these drugs on our cancer drugs A to Z list.
Chemotherapy before a stem cell or bone marrow transplant
Some people have a stem cell or bone marrow transplant from someone else. This is also known as an allogeneic transplant or allograft. Before the transplant you have treatment to prepare your body to receive the stem cells. You might hear this called conditioning treatment.
There are two main types of conditioning treatment. These are:
- myeloablative conditioning
- reduced intensity conditioning (RIC)
For myeloablative conditioning you have very high doses of chemotherapy. With reduced intensity conditioning you have lower doses of chemotherapy. You might also have other treatments such as radiotherapy to the whole body ( ).
).
The treatment kills the leukaemia cells as well as the healthy cells in your bone marrow. This makes space in your bone marrow for the donor stem cells. And dampens down your immune system so you don’t reject the donor cells.
Maintenance
Maintenance treatment aims to help keep the leukaemia away (in remission). You have more chemotherapy, but in lower amounts (doses) than in the other phases of treatment. You usually have short courses of steroids over a few days also known as pulses. You also have injections of chemotherapy every 3 months.
The drugs that you are likely to have during maintenance include:
- methotrexate
- vincristine
- mercaptopurine
- prednisolone (a steroid)
The maintenance phase lasts for about 2 years. You usually have this as an outpatient, and most people can go back to work, college or university during this phase.
Growth factors
Granulocyte colony stimulating factor or G-CSF is a type of growth factor that you might have during ALL treatment. Growth factors are natural substances that stimulate the bone marrow to make blood cells.
After chemotherapy your white blood cell count drops, so you’re at an increased risk of getting an infection. The longer your white cell count is low the greater your risk. Having a growth factor such as G-CSF helps your white cell count go up more quickly. This could lower the risk of infection.
The different types of G-CSF are called:
- filgrastim
- lenograstim
- pegfilgrastim
How you have chemotherapy
Chemotherapy for leukaemia treatment comes in many different forms. These include tablets that you take by mouth, an injection into your muscle, or a drip into your bloodstream (intravenous). You might also have it as an injection into the fluid around the spinal cord and brain.
Chemotherapy into a vein
You have treatment through a thin short tube (a cannula) that goes into a vein in your arm each time you have treatment.
Or you might have it through a long plastic tube that goes into a large vein in your chest. This might be a:
-
central line
-
PICC line
-
Portacath - although this is rare
The aim is to keep your line in place throughout the course of your treatment. Some people need to have their line replaced a number of times during their treatment. This could be because of an infection for instance.
Chemotherapy into the fluid around the spinal cord and brain
You have intrathecal chemotherapy in the same way you have a lumbar puncture. You lie on your side. Your doctor gives you a small injection to numb an area in your back. They then inject the drug between 2 of your spinal bones into the spinal fluid. It takes from 1 to 5 minutes. Afterwards you need to lie flat for an hour.
Side effects of chemotherapy
Chemotherapy for ALL can cause side effects and these can vary from person to person. It depends on the chemotherapy drugs you are having, the amount you have and if you have them with other cancer drugs. Some of the common side effects include:
An increased risk of infection
Increased risk of getting an infection is due to a drop in white blood cells. Symptoms include a change in temperature, aching muscles, headaches, feeling cold and shivery and generally unwell. You might have other symptoms depending on where the infection is.
Infections can sometimes be life threatening. You should let your doctor or nurse know urgently if you think you have an infection.
Breathlessness and looking pale
You might be breathless and look pale due to a drop in red blood cells. This is called anaemia.
Bruising, bleeding gums or nose bleeds
This is due to a drop in the number of platelets in your blood. These blood cells help the blood to clot when we cut ourselves. You may have nosebleeds or bleeding gums after brushing your teeth. Or you may have lots of tiny red spots or bruises on your arms or legs (known as petechiae).
Feeling or being sick
Feeling or being sick is usually well controlled with anti sickness medicines. Avoiding fatty or fried foods, eating small meals and snacks, drinking plenty of water, and relaxation techniques can all help.
It is important to take anti sickness medicines as prescribed even if you don’t feel sick. It is easier to prevent sickness rather than treating it once it has started.
Diarrhoea
Contact your advice line if you have diarrhoea, such as if you've had 4 or more loose watery poos (stools) in 24 hours. Or if you can't drink to replace the lost fluid. Or if it carries on for more than 3 days.
Your doctor may give you anti diarrhoea medicine to take home with you after treatment. Eat less fibre, avoid raw fruits, fruit juice, cereals and vegetables, and drink plenty to replace the fluid lost.
Tiredness and weakness
You might feel very tired and as though you lack energy.
Various things can help you to reduce tiredness and cope with it, for example exercise. Some research has shown that taking gentle exercise can give you more energy. It is important to balance exercise with resting.
Hair loss
You lose all your hair with ALL treatment. This includes your eyelashes, eyebrows, underarm, leg and sometimes pubic hair. Your hair will usually grow back once treatment has finished but it is likely to be softer. It may grow back a different colour or be curlier than before.
Sore mouth and ulcers
Mouth sores and ulcers can be painful. Keep your mouth and teeth clean; drink plenty of fluids; avoid acidic foods such as oranges, lemons and grapefruits; chew gum to keep the mouth moist and tell your doctor or nurse if you have ulcers.
Loss of fertility
Many people do go onto keep their fertility after ALL treatment. But chemotherapy can affect some people making it harder to get pregnant or father a child. Talk to your doctor before starting treatment if you think you may want to have a baby in the future.
Support at home
Chemotherapy for ALL can be difficult to cope with. Tell your doctor or nurse about any problems or side effects that you have. Your nurse will give you telephone numbers to call if you have any problems at home.



